 The elderly are often hit the hardest during flu season, and this vulnerability means that they tend to be targeted by vaccination programs. But is the whole population missing out when younger people are left unvaccinated? New research from Courtney J. Ward looks at the effects of expanding vaccination in the Canadian province of Ontario, finding that increased coverage across the entire population means that the infection rate can fall by as much as 92 percent. She argues that in order to mount the best defense against the flu, policy makers may want to ignore conventional wisdom and expand incentives for healthy young Americans to vaccinate.
The elderly are often hit the hardest during flu season, and this vulnerability means that they tend to be targeted by vaccination programs. But is the whole population missing out when younger people are left unvaccinated? New research from Courtney J. Ward looks at the effects of expanding vaccination in the Canadian province of Ontario, finding that increased coverage across the entire population means that the infection rate can fall by as much as 92 percent. She argues that in order to mount the best defense against the flu, policy makers may want to ignore conventional wisdom and expand incentives for healthy young Americans to vaccinate.
In recent flu seasons, the vaccination rate in older Americans exceeded that of healthy working age Americans two and a half times over. Even so the medical care burden for older adults still outpaced that of their younger counterparts, and millions of susceptible younger adults came down with the virus.
The disparity in vaccine take-up is perhaps unsurprising given long-standing vaccine recommendations centered on people most vulnerable to complications from the flu, e.g., older adults or those with health conditions. But new evidence suggests that this type of targeted policy misses an important piece of the puzzle. Specifically, guidelines that are based on group-specific vaccine effectiveness estimates will tell us little about the nature of an important and sizable effect: that of external vaccine benefits – the benefit passed on to others by not passing on the flu. We find that if vaccine provision is expanded across the entire population, these benefits mean that infection rates can fall by more than 90 percent.
The notion that vaccines offer benefits beyond the direct effect is not new, but without evidence on how these benefits manifest across different groups, policy makers are flying blind on how to proceed. For example, back in 2000, when the province of Ontario, Canada challenged conventional wisdom by expanding vaccine recommendations and coverage to the entire population, many saw the move as questioning the rules of evidence-based decision-making. Indeed, critics of the policy pointed to the accumulation of research showing higher benefits of vaccination in more vulnerable groups – the groups traditionally incentivized for the shot in countries around the world.
There is no arguing that flu infection in more vulnerable persons will tend towards more costly medical care. On the other hand, healthy people with stronger immune responses may enjoy a higher degree of protection from the same shot and may leverage that protection over a larger network of people. So while flu infections will cost more in vulnerable groups, vaccination of healthier individuals may pass on external benefits at a higher rate. Ironically, this means that the size of external benefits across the group will run counter to the size of traditional estimates of vaccine effectiveness, and it also suggests that by focusing incentives solely on the most vulnerable groups, we might find everybody loses out overall.
Fortunately, even though the Ontario flu program went against existing evidence on vaccination targeting, it gave back by providing years of evidence on flu epidemics under a policy of universal coverage – a history that can help us understand the impact of a universal approach to vaccination policy. Naturally, the policy impact for vaccine take-up and overall health benefits is of primary interest. But even more crucially, we might be interested in whether universal coverage affects the distribution of externality benefits, whether benefits decline to exhaustion at higher vaccination rates, and whether any of these effects depend on the match of the vaccine season-to-season.
To get a sense of impact of the program on vaccine take-up, we can start by comparing the post-program change in vaccination for cities in Ontario (where the policy change occurred) versus other Canadian cities (where vaccine policies remained the same). The results given in Figure 1 show that Ontario’s cities had a comparative increase in take-up in younger age groups (age 10-65) and no difference for older adults (age 65+). Thus, we see that the program effect is centered on the age groups affected by the change in coverage: a relative increase of about 11 percentage points for the young and no change in the old.
Figure 1 – Post-2000 Change in Vaccination Rates for Flu Seasons Spanning 1995-2005 in Canada
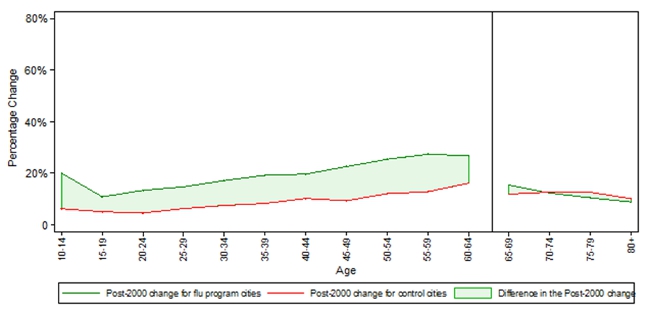
Notes: The figure shows the change in vaccination in the pre period (season 1995/96 to season 1999/00) versus post period (season 2000/01 to season 2005/06). Rates are based on data from the master files of the National Population Health Survey Cycle 2 and the Canadian Community Health Survey Cycles 1.1, 2.1, 3.1.
But the real question here is whether this had any impact on health outcomes, and in the case of work absences and hospitalizations, the results show a sizable effect. In seasons delivering a well-matched vaccine, Ontario cities saw a much higher relative gain compared to other Canadian cities: there is 14 percent less work absence and 48 percent less flu-pneumonia hospitalizations (this is after controlling for other confounders such as differences across cities and season, and post program differences in Ontario that were not due to the flu program).
In the face of such large effects, we might consider whether external benefits accrue, and particularly, whether these benefits are delivered across age group. For instance, since there is no relative gain in vaccination for older adults, we would expect to see no relative gain in health outcomes… that is, unless older adults are affected by vaccination of the young. To see how older adults in Ontario fared post-2000, Figure 2 plots baseline hospital admission rates for flu-pneumonia against the flu program effect in the case of a well-matched vaccine. Results show that the post-2000 increase in vaccination for Ontario’s young led to much higher relative gains across all age groups. So even though there was no relative change in vaccination for older groups, Ontario’s seniors enjoyed an additional 25 percent decline in admissions for seasons that delivered a well-matched vaccine. Since the rates of hospitalization are highest among older adults, this represents a sizable effect in terms of numbers of hospitalizations averted.
Figure 2 – Flu and Pneumonia Admissions in Flu Season: Baseline Admission Rates and Percent Decrease due to the Universal Flu Program
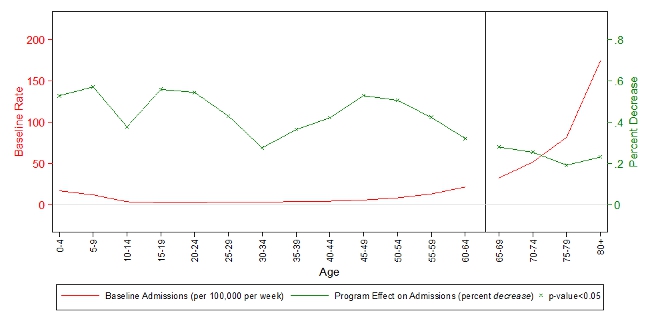
Source: Author calculations and hospitalization data from the Hospital Morbidity Database.
How big are these excess effects overall? One benchmark to consider is the percent decrease in the number of unvaccinated people. With a bit of math we can show that if excess benefits are zero, the percent decrease in the number of unvaccinated people would equal the percent decrease in the flu infection rate (i.e. the overall probability of infection falls only because we changed the composition of vaccinated and unvaccinated groups).
However, comparing these two numbers, we find that the 11 percent decrease in the proportion of unvaccinated people was dwarfed by the percent decrease in the infection rate. For example, considering the best-case scenario of a well-matched vaccine, the overall decrease in the infection rate was as high as 92 percent. So in this instance, there are large excess benefits from universal coverage, suggesting significant advantages to developing well-matched pandemic vaccines (e.g. the 2009 H1N1 vaccine) and considering strategies (both in research and policy) that do not overlook the size of external effects.
Is there a limit to the benefits of further vaccination? In effect, if we think external benefits matter, then scaling the vaccination rate will eventually lead to decreasing returns. Theoretical models of infectious disease, for instance, suggest that a vaccination rate greater than 31 percent would completely prevent a flu epidemic. Here, we can think of each flu infection as a lit match in a wet forest; the forest fire never has a chance to take off.
Since vaccination rates in Ontario jumped to more than 40 percent, according to the theoretical literature, the changes in vaccination occurred within the most effective range possible. Testing this theory in the Ontario case, delivers a similar conclusion; post program benefits for work absences and hospitalizations would be exhausted at vaccination levels in the mid 30’s. Importantly, though, this final result depends on the compositional take-up of vaccination in the population, which will go on to leverage external benefits at a different rate.
The bottom line here is that contrary to the conventional literature, which ranked vulnerable groups as the most cost effective target, expanding incentives for healthy young people to vaccinate might be the better strategy of defense against flu and its associated medical costs.
This article is based on the paper ‘Influenza Vaccination Campaigns: Is an Ounce of Prevention Worth a Pound of Cure?’, in the January 2014 issue of the American Economic Journal.
Please read our comments policy before commenting.
Note: This article gives the views of the authors, and not the position of USApp– American Politics and Policy, nor of the London School of Economics.
Shortened URL for this post: http://bit.ly/1jGUZVB
_________________________________
 Courtney Ward – Dalhousie University
Courtney Ward – Dalhousie University
Courtney Ward is an Assistant Professor in the Department of Economics at Dalhousie University, Halifax, Nova Scotia, Canada. Her research interests include applied microeconomics, health economics and labour economics. Her research focuses on the implications of externality and selection effects in health production, and her work has particular emphasis on how these aspects interact with policy in intended or unintended ways.




The flu vaccine was 18% effective last year. A vaccine that is ineffective is not worth taking. The risk benefit ration is poor. Never take a flu shot. They are useless.