
 In one London NHS trust, one in five nurses are from the European Economic Area. Rachel Marangozov and Matthew Williams explain why some parts of the NHS have become increasingly dependent on the EU migrant workforce and look at the implications of Brexit on recruitment. With ongoing shortages and so many nurses due to retire over the next decade, the government needs to act now to ensure we have enough nursing staff.
In one London NHS trust, one in five nurses are from the European Economic Area. Rachel Marangozov and Matthew Williams explain why some parts of the NHS have become increasingly dependent on the EU migrant workforce and look at the implications of Brexit on recruitment. With ongoing shortages and so many nurses due to retire over the next decade, the government needs to act now to ensure we have enough nursing staff.
The composition of the overseas nursing workforce has shifted dramatically in recent years; nurses from the European Economic Area (EEA)[1] are now increasingly prevalent, reflecting a change in recruitment practices due to tighter immigration rules, fewer employment opportunities across the Eurozone and health sector employers seeking to bring in more migrant nurses in general to alleviate shortages.

Nurses from the European Economic Area currently make up 4.5 per cent of the total nursing workforce in England. That may not sound like a lot, but it masks huge geographic differences between NHS Trusts, with some much more reliant on this recruitment pipeline from Europe than others because of current nursing shortages. Brexit threatens this labour supply because of the continuing uncertainty surrounding the status of EU workers in England, which makes it harder for Trusts to recruit from Europe as well as to retain current EEA nurses already working here who might well be questioning their future prospects in the UK. The Royal College of Nurses has already called on the government to secure the future of all EU nurses working in the UK.
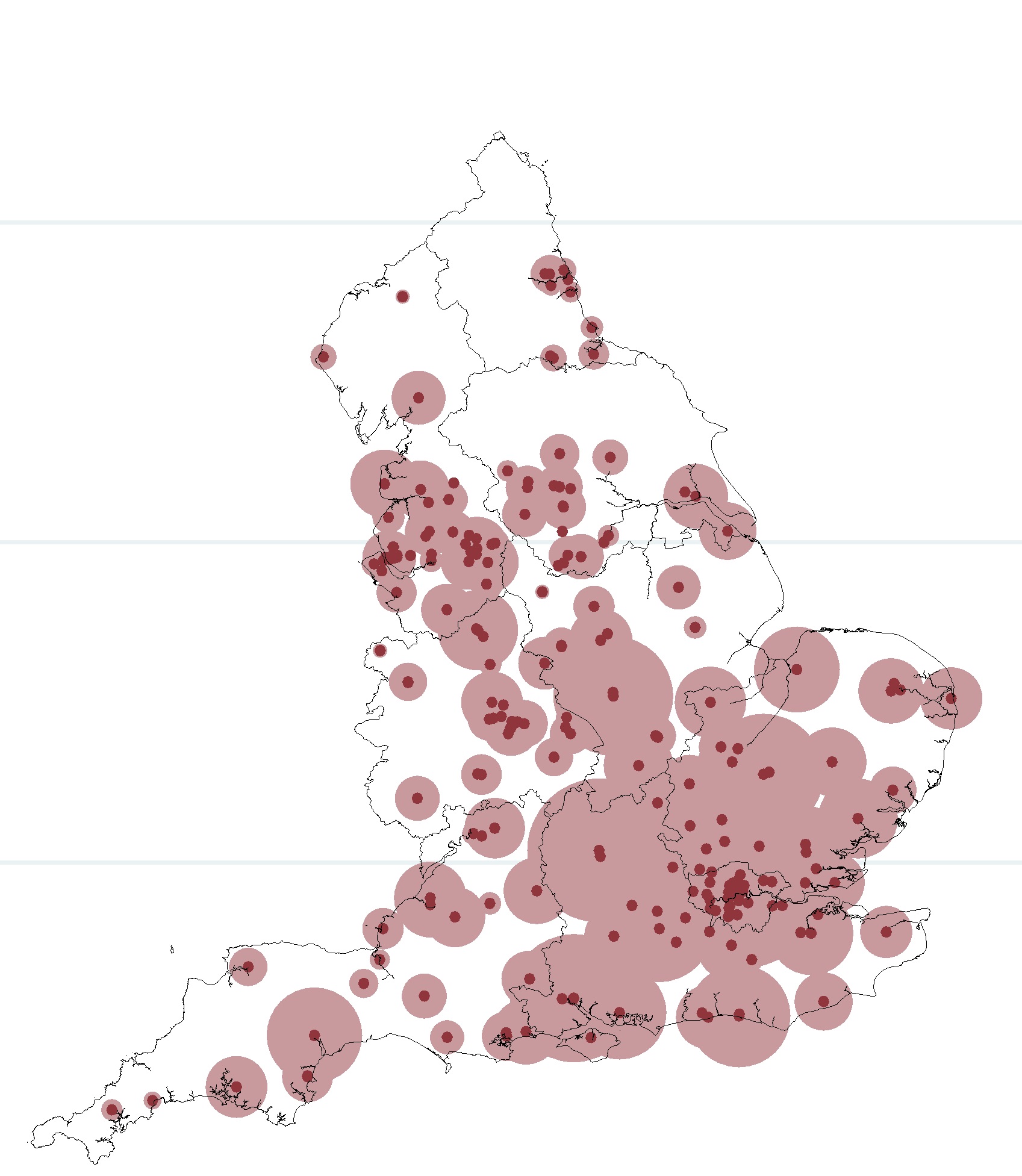
New data analysis by the Institute for Employment Studies reveals that NHS Trusts in the London, Thames Valley and the East of England regions are most likely to be affected by Brexit because they are the most dependent on the recruitment pipeline from Europe. The map of England below show the locations of trusts that have the largest stock of EEA nurses during the period 2009 to 2015, with circles proportional to the total number of EEA nurses. The figures show that the concentrations of EEA nurses are highest in trusts located in the South East of the country, and particularly those located in London.
The data shows that particular NHS Trusts are likely to feel the ‘pinch’ more than others. For example, in Royal Brompton and Harefield NHS Foundation Trust, 20 per cent of their nurses are from the EEA; similarly in Queen Elizabeth Hospital King’s Lynn NHS Foundation Trust, 18 per cent of their nurses are from the EEA. Queen Elizabeth Hospital King’s Lynn also saw the largest increase in the use of EEA nurses, with the proportion increasing from just 1.3 per cent in 2009. Other trusts that experienced large increases in their proportions of EEA nurses are Papworth Hospital NHS Foundation Trust and North Middlesex University Hospital NHS Trust.
But how much of a problem is this, and what are the alternative sources of nurses available to the NHS?
The answer to the first question came from the Migration Advisory Committee in March 2016, when they reported that nursing vacancies in some Trusts were as high as 10 per cent and recommended that the government issue 15,000 visas over the next three years to nurses from outside of Europe to ease the current workforce pressures. Since then, further research has highlighted the longer-term nature of nursing shortages, revealing that one in three nurses in England are due to retire in the next ten years and that demand for nurses (and healthcare services more generally) are only due to increase over this period. [2] Arguably, then, Brexit couldn’t have come at a worse time, potentially restricting the supply of European nurses when many NHS Trusts need them the most.
Of course it is possible to recruit more nurses from outside the EEA. International nurses, from countries like India and the Philippines have always played an important role in the NHS, and continue to do so, making up eight per cent of the total nursing workforce in England. In March of this year, the MAC put nursing on the Shortage Occupation List for three years, making it easier for NHS Trusts to recruit from outside of Europe. The MAC’s recommended 15,000 visas will undoubtedly ease the immediate to short-term pressures on the NHS but this will not be enough to make up for the loss of a third of the nursing workforce to retirement over the next ten years.
The most sensible solution now, particularly post Brexit, would be for the government to act now to ensure that we have a ‘homegrown’ domestic supply of nurses. This will require adequate and sustained investment in workforce planning to address the potentially gaping hole in our future nursing workforce. For too long now, there has been a lack of long-term, strategic workforce planning that offers oversight, coordination and alignment of the different dimensions of the nursing workforce (financial, education, employment and international recruitment).
For example, workforce planners have known for several years now that the ageing nursing workforce is a problem, and yet very little, if anything, has been done about it; and in recent years there has been a lack of student nursing training places despite demand for nursing courses outstripping supply. In 2014, some 30,000 applicants, or more than 60 per cent of total applicants, were not successful in obtaining a funded place on pre-registration courses, so we are not short of people interested in becoming nurses! It is time that workforce planners in the government make the most of this potential and avoid using overseas recruitment as a ‘quick fix’ to nursing shortages in the UK, while ignoring more systemic workforce planning issues.
[1] The EEA includes all European Union (EU countries) and also Iceland, Norway and Liechtenstein.
[2] Marangozov R., Williams M. And J. Buchan (2016), The Labour Market for Nurses in the UK and its relationship to the demand for, and supply of, international nurses in the NHS. Institute for Employment Studies.
This post represents the views of the authors and not those of the BrexitVote blog, nor the LSE.
Rachel Marangozov is a Senior Research Fellow at the Institute for Employment Studies and a Fellow of the LSE.
Matthew Williams is a Research Fellow at the Institute for Employment Studies.






Just give them Amestey !