Vaccine uptake protects individuals and societies, but how much is the COVID-19 vaccine worth? Joan Costa-Font (LSE), Caroline Rudisill, Sayward Harrison (University of South Carolina), and Luca Salmasi (Università Cattolica del Sacro Cuore) estimate that the willingness to pay for a COVID-19 vaccine in the US, UK, Spain, and Italy in July 2020 ranged between 100 and 200 US dollars. However, the social value of the vaccine exceeds its market value.
Vaccinating the population against COVID-19 does not provide individual self-protection but benefits the wider society by increasing the chances that it will attain herd immunity, reducing hospitalisations, and allowing the economy to bounce back to normal. In other words, vaccines give rise to positive externalities for population health, society, and the economy. Vaccine availability does not, however, necessarily entail widespread vaccination demand as a share of the population might be unwilling to vaccinate. Multiple SARS-CoV-2 vaccines have been found to be safe and produce a sufficient immune response to gain approval for wide vaccination with very few exclusionary criteria. However, the value of a vaccine to individuals and society is affected by individual perception on multiple levels (e.g., the vaccine itself, the development process, regulatory agencies). Hence, the population perceives a social value of vaccination, and this social value depends, in part, on individual level preferences.
Determinants of vaccine uptake
- Individual traits: There are some important individual level determinants of vaccine uptake. For instance, risk-seeking and less pro-social individuals (Betsch et al. 2013) are less likely to vaccinate, and women are generally less likely to support vaccination than men.
- Knowledge: Limited knowledge of what vaccines do, and opposition from trusted sources (e.g., family and friends) has been shown to play an important role in some countries (Rainey et al. 2011).
- Trust: Another important factor that impacts vaccine hesitancy is trust in medicine and healthcare providers, which varies across socio-demographic groups and country. Trust in information from governments has been shown to be positively related to SARSCoV-2 vaccine acceptance in a 19-country survey. Similarly, trust with key stakeholders such as the WHO and health care systems may be especially important. An environment of distrust in institutions and “experts”, additionally, can hamper the public acceptance of vaccines.
- Trusted information gatekeepers: Evidence suggests that trust in healthcare professionals has a key role in attitudes to vaccination. Health care professionals are trusted gatekeepers in some countries. However, in some cases they are part of the problem as they might well be steering vaccine hesitancy among the population. Other trusted gatekeepers include community leaders and in some cases celebrities, when their actions are emulated by the population.
What is the social value of a COVID-19 vaccine?
The social value of a COVID-19 vaccine exceeds its market value. In a recent paper, we estimate the willingness to pay (WTP) for a hypothetical SARS-CoV-2 vaccine in four countries, namely the US, the UK, Spain, and Italy, during the first wave of the COVID-19 pandemic, when no specific vaccine had been approved nor subsidised. WTP estimates are elicited using a payment card method. Our estimates suggest that the average value of a hypothetical vaccine is 100-200 US dollars once adjusted by purchasing power parity (PPP). Figure 1 below reveals a higher willingness to pay by younger and more affluent individuals, those who had COVID-19, and those who have children. WTP estimates are lower in the US than in most European countries.

Figure 1: Correlates of WTP for a COVID-19 vaccine (US$)
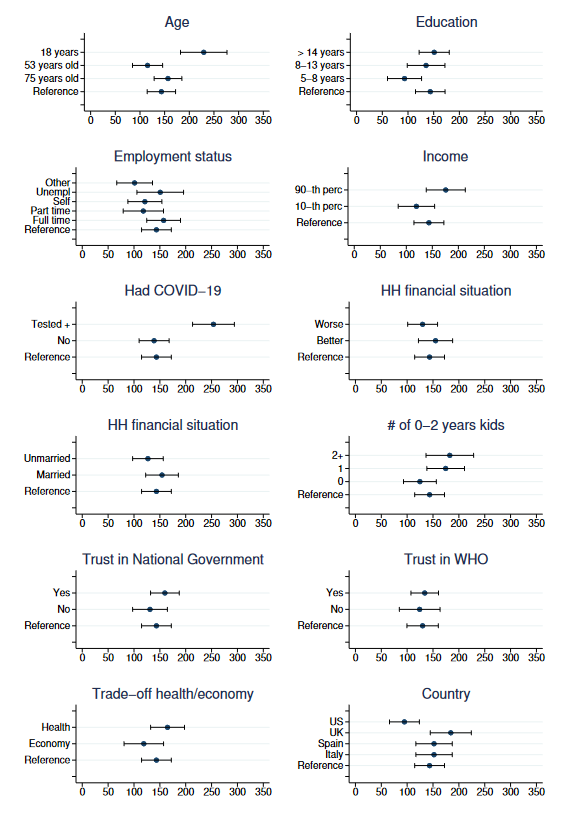
Findings demonstrate no variation between Spain and Italy, but higher values in the UK and lower values in the US, compared to the other countries. However, back in summer 2020, the estimated WTP for a vaccine in the US results in part from respondents’ mistrust in the national government, since people who trusted the US government declared a WTP equal to that of respondents in other countries.
WTP estimates seem to be sensitive to personal experiences with COVID-19. Notably, we find that individuals who have been sickened by the virus are willing to pay significantly more than those who have not been infected.
The social value of a vaccine exceeds any price value
These findings suggest that the social value of a SARS-CoV-2 vaccine is considerably larger than the actual price of any vaccine, which indicates that vaccines encompass significant welfare improvements. Our results justify full vaccine subsidisation in the context of COVID-19, and even to some degree incentives for vaccine uptake, given the externalities it engenders for everyone else in the economy, and more widely in society. These findings are important for policy makers in understanding the societal value of the SARS-CoV-2 vaccine in the absence of individual level purchasing decisions.
This post represents the views of the authors and not those of the COVID-19 blog, nor LSE.
This post is based on The Social Value of a SARS-CoV-2 Vaccine: Willingness to Pay Estimates from Four Western Countries, IZA Institute of Labor Economics, June 2021. It first appeared at the LSE Business Review blog.