 Delivering fresh insights on evidence-based practice, Ben Hannigan charts how a combination of action research and qualitative methods helped identify the role of ‘critical junctures’ in improving mental health services and practitioner support. This analysis helped to connect people, processes and systems and was able to overcome the ‘micro’ and ‘meso’ distinctions holding back longer trajectories of care and change.
Delivering fresh insights on evidence-based practice, Ben Hannigan charts how a combination of action research and qualitative methods helped identify the role of ‘critical junctures’ in improving mental health services and practitioner support. This analysis helped to connect people, processes and systems and was able to overcome the ‘micro’ and ‘meso’ distinctions holding back longer trajectories of care and change.
Many people experience difficulties with their mental health. Over 16% of adults participating in a major household survey in England in 2007 met the criteria for at least one common mental disorder in the week prior to their taking part. Most who receive help do so through primary health care. Smaller numbers use secondary services provided by specialist interprofessional teams, which can be based either in the community or in hospitals. In my earlier career as a practitioner I have worked in teams of this type, and with colleagues in Cardiff and beyond I now study them and the larger systems of which they are a part.
What particularly interests me are the interrelationships between mental health policy, the organisation of services, the work that people do and the experiences of users. Funding for research in these areas is often targeted at projects which set out to produce new knowledge of practical use to managers and professionals with primary concerns in finding out how care can be improved. As I have recently found, bringing together observations from otherwise unconnected studies in this broad field can add significant value to what can be learned from single projects alone.

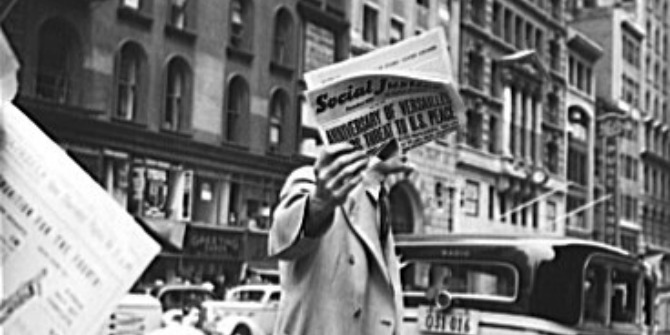
In an article published in Social Theory & Health my colleague Nicola Evans and I show how free-flowing conversations, ranging over different sets of data, can lead to unexpected but very welcome insights. Nicola used action research methods to introduce a novel service innovation in a community child and adolescent mental health team as a way of improving the management of demand and reducing waiting times. I used qualitative methods to investigate the establishment, work and wider impact of a crisis resolution and home treatment team providing a community alternative to psychiatric hospital admission, and to explore the experiences of users.
In my study I gathered data relating to people’s journeys into, through and out of crisis care, and relating to the work of practitioners during these periods. Episodes of acute mental ill-health are major events for the people experiencing them, and in organising service responses workers have to make decisions. In talking about my data with Nicola the thought occurred to us that, at certain points, decisions have magnified importance. They may set service users and the staff surrounding them along particular paths, and may involve bringing people into new parts of the wider system.
In her study Nicola was less interested in studying pivotal moments of this type than in making narrative use of them as a means of promoting larger organisational change. In her fieldwork Nicola encountered a young person who had waited many months for a specialist mental health appointment. When members of the team finally met this person their decision was to urgently mobilise services in recognition of her significant need. Nicola recounted this story to the team she was working with as a means of encouraging their adoption of a new and quicker way of screening referrals.
Talking about our respective datasets, and doing some new reading, led us to cross-disciplinary social scientific ideas concerned with the study of turning points. We have (re)introduced some of these into the health and social care context though an analysis of what, in our article, we call ‘critical junctures’. We have discovered that the language of ‘critical junctures’ features prominently in the study of political history, where it refers to moments of heightened significance for whole nations or territories. In our paper we first take this idea all the way down to the level of the single individual and those immediately surrounding. At this far more microscopic scale we refer to ‘critical junctures’ as ‘temporally bounded sequences of events and interactions which alter, in lasting ways, both the personal health and illness experience and the caring work which is done’. We suggest that critical junctures initiate (or take place within) longer trajectories of care, and the decisions that are made during them can propel people and processes in directions which may be hard to reverse. We use detailed data from my crisis services study to illustrate this thinking, drawing in particular on a single service user’s experiences and her entry into (and journey through) the system.
To show how small-scale critical junctures can assist change at larger scales of organisation we then use observations from Nicola’s action research project. We cite her example of an individual critical juncture being told as a story to help a whole team in its search for a new, and better, way of working. In the case of the mental health team Nicola worked with in her study this meant adopting a triage clinic, through which newly referred young people could be effectively, efficiently and safely screened for evidence of mental ill-health.
Preparing our article reminded us of a simple truth: that conversations between colleagues, in which studies with unrelated sets of data are traversed, is a means of fostering new insights. When academics have their heads down trying to complete single-project reports for funders this kind of talk may not happen as often as it might. Writing our paper also reminded us of the benefits to be had by crossing disciplinary boundaries. We blend ‘turning point’ ideas from a number of social scientific traditions (sociology, political history, complexity science – which itself is something of a hybrid), and carry these into the specific context of mental health services. Using these as a lens through which to view individual and organisational-level data from two projects enabled us to make new connections between people, processes and systems spanning the ‘micro’ and the ‘meso’ scales.
Note: This article gives the views of the author, and not the position of the Impact of Social Science blog, nor of the London School of Economics. Please review our Comments Policy if you have any concerns on posting a comment below.
Ben Hannigan is a Reader in Mental Health Nursing in the Cardiff School of Nursing and Midwifery Studies. He is interested in mental health policy, services, work and roles and in the experiences of users. He has written widely in these areas in health, nursing and social scientific journals, and blogs about his work (and other things) at http://benhannigan.com






2 Comments