Latin America’s coronavirus outbreak is playing out against a backdrop of already rampant arboviruses like dengue, chikungunya, yellow fever, and Zika. Global guidelines on tackling Covid-19 fail to take into account local specificities, underplaying especially the social risk factors underlying this “syndemic”. With the Brazilian health system in particular danger of being overwhelmed, the vital work of community health workers must be protected at all costs, write Clare Wenham (LSE Health Policy), Gabriela Lotta (Fundação Getulio Vargas), and Denise Pimenta (Fundação Oswaldo Cruz).
• Também disponível em português
Dengue fever, Zika, and now Covid-19 are all global health challenges that collectively amplify each other’s impact on public health. Going beyond notions of “comorbidity” or “cross-epidemics“, this “syndemic” is a ticking time bomb for Latin America.

Global guidelines for a Latin American syndemic?
The term syndemic implies a complex web of social and environmental factors that promote and enhance the negative effects of disease interaction. In the case of mosquito-borne diseases in Latin America, the same places where mosquitoes breed are those where Covid-19 will hit the hardest. Poverty, low education levels, high population density, lack of sanitation and sustainable access to water, lack of access to health services, poor housing and waste management, and gender inequalities can all reinforce the social reproduction of disease.
There have been some concerns raised, for example, about the public health interventions demanded by the World Health Organization.
Recommendations to wash your hands for 20 seconds are futile if there is no water to wash anyone’s hands. Asking populations to self isolate is only possible if they have homes in the first place. Social distancing is difficult if there are 10 to 15 people living in a house or if that house is poorly built and lacks structural walls. How are people to stay at home if their daily economic stability depends on informal labour? And what about those beyond the edges of the social safety net, uncounted by government structures and calculations?
These are very real considerations for many in Latin America, and particularly the people of Brazil. Aside from the inadequacy of global recommendations that overlook local contexts of vulnerability and inequalities, Covid-19 also overlaps with a number of other health conditions and tropical neglected diseases.
The coronavirus-arbovirus syndemic in Brazil
In Brazil, Covid-19 comes on top of a major dengue epidemic. Worse still, this epidemic itself arrived on the back of the Zika crisis in 2016, the introduction of chikungunya fever, and a major yellow fever outbreak in 2018.
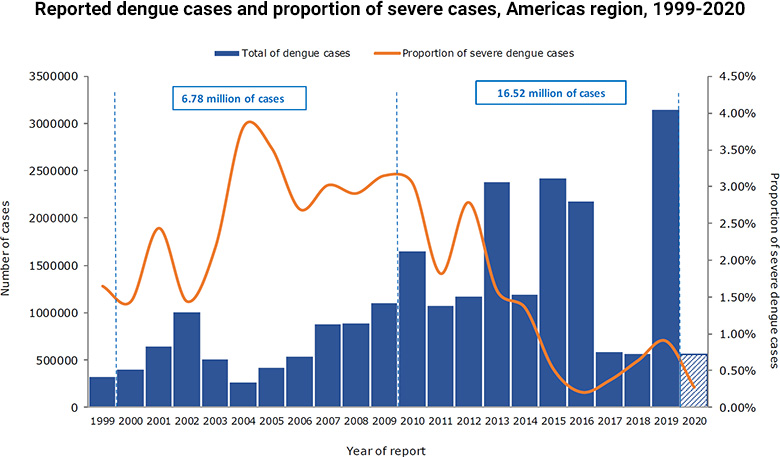
As Covid-19 has unfurled across Latin America, Brazilian authorities have continued to underpin the importance of Covid-19 in the context of dengue fever, which in 2019 saw its highest ever total of recorded cases in the Americas (3.14 million). In 2020, there have already been over a half a million reported cases in Latin America.
Cases of these arboviruses, spread by Aedes aegypti mosquitoes, have skyrocketed in recent years. Despite a number of government interventions to limit their spread, none has managed to do so sustainably. The need to mitigate Covid-19 whilst simultaneously providing routine vector control and caring for those infected with arboviruses could easily stretch the Brazilian National Health System (SUS) beyond its limits.
If modelling of Covid-19’s spread is accurate, the latest estimations suggest that the SUS will be on the brink of collapse in April 2020, the same month that tends to see the annual peak incidence of dengue fever.
The vital role of community health workers
Key to interventions against mosquito-borne arboviruses is the role of community health workers and vector control agents.
Community health workers visit homes to provide health services directly to inhabitants and to deliver clinical information on public health risks to those at greatest risk of infection. Vector control agents, meanwhile, undertake larger-scale fumigation and mosquito-reduction strategies in homes and civic spaces. These workers act in a territorialised way, visiting homes and interacting intensively and actively with communities. More recently, they have also been delivering information on Covid-19 and providing access to primary health services.
Last week the Brazilian Health Ministry published specific Covid-19 guidelines for community health workers and vector control agents, asking them to support community engagement and preparation for the outbreak. This meant providing guidance and communication on hand washing and social distancing, as well as identifying new cases and reporting them to public health surveillance teams.
There is, however, a tension between public health recommendations on physical distancing and community health workers’ need to interact directly with communities to control the coronavirus Covid-19 and also arboviruses like dengue, Zika, and chikungunya. Moreover, these (largely female) community health workers are not being provided with personal protective equipment (PPE) or relevant training, which leaves them at risk of infection during direct engagement with communities. As such, it is likely that some will be unable to continue their work, either because they are self-isolating or through a reluctance to expose themselves to this heightened risk.
Gangs, governance, and vector control
On top of this, the emerging territorial governance in some favelas has seen gangs policing entry into their territories and implementing curfews to minimise the potential for transmission. We know from the Zika outbreak that gangs can control access to health care, including if and when community health workers or vector control agents are allowed to be present. This phenomenon is likely to be amplified during the Covid-19 crisis.
The biggest worry here, beyond an explosion of the Covid-19 outbreak alone, would be a simultaneous surge of dengue fever, chikungunya, yellow fever, and Zika due to the degeneration of community vector control. This kind of convergence would almost certainly cripple the SUS and cause a major national crisis for decades to come.
As has occurred repeatedly in the past, health emergencies can distort health activities more broadly: the entire focus of the health system is often hijacked by the need to respond to the immediate crisis. Meanwhile, routine areas of health care – such as endemic disease control, maternal care, and childhood immunisation – end up overlooked, unfunded, and unimplemented.
A call to action
Given our existing knowledge about how such breakdowns occur, we call on governments and international organisations to recognise and respond to the competing challenges presented by arboviruses during the coronavirus crisis. Together national, regional, and global institutions must ensure that community health workers and vector control agents are not only fairly compensated for their work but also properly protected through provision of suitable personal protective equipment.
If Latin America manages to defuse this public health time bomb, it will be thanks in great part to the unsung efforts of these workers in protecting communities from the spread of Covid-19 and maintaining vector control activities against dengue, chikungunya, yellow fever, and Zika.
Notes:
• The views expressed here are of the authors rather than the Centre or the LSE
• Please read our Comments Policy before commenting





