Pandemics have long aftermaths and epilogues; they leave an imprint in history even if this was ignored by contemporaries. The responses to prevent or control them may change the way we live, our relationship with others and the state long after the outbreak has passed, write Kah Seng Loh and Li Yang Hsu.
_______________________________________________
Writing a history of infectious diseases against the backdrop of COVID-19 offers a certain challenge for the historian, but also a vital opportunity. The tone, emphasis and ‘learning points’ from such a work would have been quite different if there had been no coronavirus pandemic, or if it were written before the advent of the emerging infectious diseases in the last 20 years. The idea of learning from history is a challenge because it raises questions about the relationship between the past and present that go to the heart of the historical discipline. But it is also an opportunity to bring epidemic disease to the study of the past, and for historians to think long and hard about how they can draw upon their work to inform social issues.
History is also about context and the particular: it is about this person or that event in a specific time and place. Singapore, as a tiny developed nation-state and port city in Southeast Asia, presents similarly a limitation and a strength. Shorn of a physical hinterland, its experience appears to speak little to bigger countries with multiple urban settlements and large rural areas. Its history may also seem unhelpful for states lacking the governance, infrastructure, technology, or multicultural population that Singapore possessed.
However, what the island of a mere 700-odd square kilometres does offer is an excellent case of micro-history. Pandemics are by definition international events but their histories are also a sum of local events, trajectories and actors. By tracing Singapore’s epidemiological pasts in depth, we derive a sense of the experiences, consequences and responses of an urban population’s openness to the world, including the world of microbes. This provides the context for considering how a history of pandemic disease may be useful for preparing for future threats.

Pandemics in History
There are only a handful of accounts of pandemics that have tried to explain why. Most of these, save for a select few, are not widely read. The first step to remedy this is to recognise that pandemics are an integral part of human history, even though unlike infectious diseases, they are fairly rare events. Pandemic should be written into general historical narratives. We also ought to note that widely spreading disease outbreaks are becoming more frequent as the world becomes ever more inter-connected and humans have an increasing impact on the ecological system. While it is vital to write historical accounts of pandemics, it is just as important for historians to include infections and pandemics in their work where it is relevant to do.
Pandemics are inherently historical. We can speak of their immediate causes (or catalysts), long-term causes or variety of causes. George Dehner notes that influenza pandemics have become more probable over the course of human history because people have been living in increasingly dense communities that are closely interconnected with other such communities. As this form of human settlement became more prevalent particularly from the 19th century, , it is not surprising that influenza pandemics have increased in frequency and virulence.[1]
As Mark Honigsbaum observes in his survey of 20th century pandemics in the midst of the coronavirus crisis, it is neither possible nor desirable to predict the next pandemic. Advances in medical science have ironically locked scientists into self-limiting paradigms and theories. The last pandemic has tended to create a hypervigilance about a specific disease or group of pathogens, but this can cause misdirection and error. Honigsbaum’s point is a timely one: would the COVID-19 episode trigger a similar overemphasis on coronaviruses? He argues that it is more useful to explore the ecology of infectious diseases, which points to the effects of long-term environmental and social developments such as rising globalisation and urbanisation.[2]
Pandemics are also historically significant events. They have an immediate impact on human lives, families or components of human society such as the economy or the culture. In this, the insights afforded by social history are indispensable yet they have often been ignored. In her excellent book Pandemic 1918, Catherine Arnold retraces the influenza pandemic in the West through the eyes of those who experienced it first-hand – ‘East End schoolgirls, Mayfair debutantes, Boston schoolboys and Italian immigrants’.[3] Pandemics narrated this way compel historical accounts to move away from the great men (including leaders and doctors) to the little people who bore its full brunt. The scale of infection and deprivation should help communities and societies remember and commemorate their epidemic pasts. Social memory is a key resource in preparing for the next pandemic.
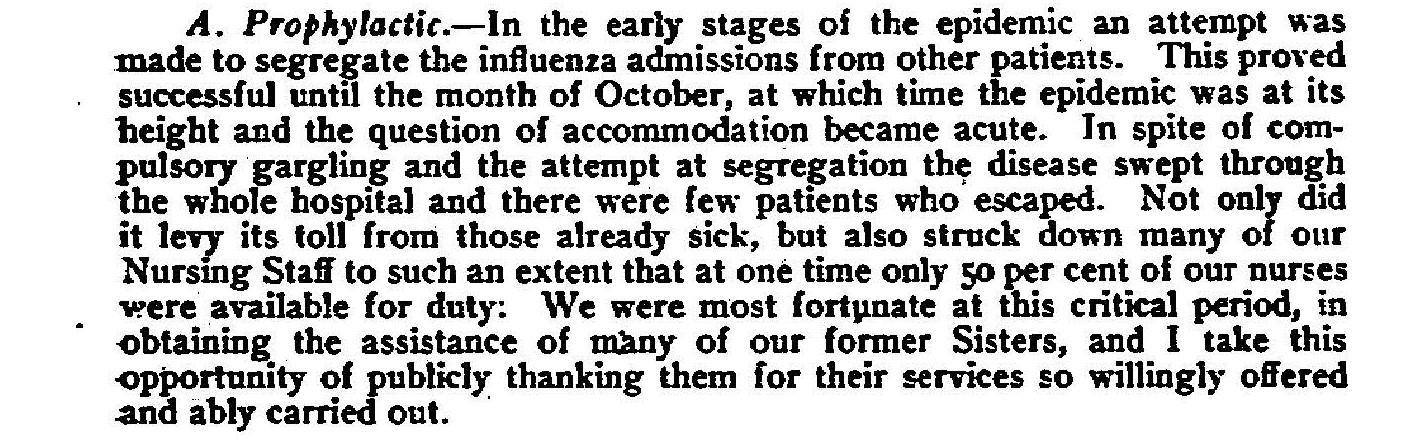
Moreover, pandemics have long aftermaths and epilogues; they leave an imprint in history even if this was ignored by contemporaries. The responses to prevent or control them may change the way we live, our relationship with others and the state long after the outbreak has passed. Or a modern pandemic could be important when it fails to elicit the active responses that have become synonymous with the Severe acute respiratory syndrome (SARS) and COVID-19 pandemics. In Britain, the 1918 influenza pandemic unravelled major failings on the part of the government and medical establishment, with both appearing to have done little in the face of the epidemic. Senior officials were defensive, insisting that they could not have anticipated, prevented or halted the spread of the illness. This can be explained by the period of transition the country was undergoing, with new emphasis on individual rights and calls for a less intrusive government. The medical experts, too, were divided over the causal agent and the ways to combat the outbreak.[4]
Finally, pandemics have another connection with the past when they are recalled or commemorated. One of the questions we try to address is why certain pandemics are widely remembered while others are pushed to the fringe of social memory. According to Peter Furtado, the 1918 influenza pandemic that ravaged much of the globe was a ‘strangely private affair’; while masks were worn in certain places, there was no lockdown and relatively little media coverage.[5] While influenza has been called the ‘Blue Death’ due to its outward manifestations, this is much less known than the original version of the term, the ‘Black Death’ commonly used for plague.

Through Niall Johnson’s research, we see that the 1918 pandemic in Britain largely slipped away from national, local and family histories and memories, overshadowed by the horror of the First World War. Its wider historical effects on demographic trends, family formation, the healthcare system, and on politics, also appear limited. Notably, in only a few countries such as Brazil, Samoa and South Africa did the 1918 tragedy shake the political leadership or order.[6] With upper estimates of 50 million deaths, it is quite incredible that the event had become ‘little more than a sad footnote to the more public tragedy of the Great War’.[7]
At the same time, historical research encourages us to read dominant accounts and official sources more carefully. The outbreak of disease on a massive scale often triggers social fault-lines and reveals blind spots. Pandemics are lived through and experienced very differently according to where people stand on the categories of class, ethnicity, gender, or age. When a case of mass infection, suffering and death during a pandemic is ignored and forgotten, as has been claimed about the passing COVID-19 epidemic in the US today, there is something to be said about whose lives mattered (or did not matter) and to whom.[8]
Asian and Colonial Contexts
The literature on pandemics is overwhelmingly Eurocentric, despite the fact that many outbreaks, including the present one, have Asian origins, trajectories, impacts, responses, and contexts. Part of the reason is due to the paucity of sources in many Asian countries, both in the colonial and post-colonial years. When many of these countries were under foreign rule, their archives comprised colonial records written from Western vantage points, while their post-colonial archives may remain fragmentary or have become difficult to access. The challenge is to unearth Asian perspectives and narratives from the available sources, while taking into account the impact of colonialism and Asian responses on the pandemic experience.
Colonial histories of medicine in Asian countries tend to be more critically oriented towards power than standard Western accounts of pandemics. This has given rise to a view of biomedicine as a ‘tool of empire’. In his classic work, Colonising the Body, David Arnold conceptualises the history of biomedicine in British India as one of the colonisation of Indian bodies in addition to territories. Biomedicine was thus an integral part of the colonial system. Arnold also uncovers Indian resistance as a key part of the history,[9] which differs markedly from the more egalitarian social history of pandemics that Catherine Arnold and others have written. The relationship between people and the state in many colonial histories is that between foreign rulers and subjugated natives.
To trace the history of Western medicine in India is, David Arnold suggests, to investigate the colonial artifice itself and the mediating influence of local circumstances and medical traditions. In what has become a theme in colonial medical histories, he highlights the ordering and othering of people into immutable races during disease outbreaks. Western doctors held that Indians were more vulnerable to disease and attributed this to undesirable cultural practices.[10] Following our previous work on tuberculosis, our research records instances of racial commentary during Singapore’s pandemics on a society that was more ethnically diverse than in India.[11]
Another classic example of the ‘tools of empire’ approach is Lenore Manderson’s Sickness and the State on British medical policy in Malaya. She writes, ‘Tropical medicine was a cultural construct, the scientific stepchild of colonial domination and control’.[12] As with David Arnold, she maps a medical pluralism in colonial Malaya. Biomedicine was only one of several medical systems there, contending and interacting with the healing traditions of the various Asian groups. This medical pluralism has also been uncovered in colonial Africa.[13] This dive into social and cultural history is fruitful in multiracial Singapore.
At the same thing, it is important to recognise that colonialism, long-term causation and the ecological approach are not mutually exclusive: they all affect each other. More recent works on India have shown how British understanding of the risk posed by infectious diseases was shaped by international debates and perspectives as much as local situations. Colonial health interventions were not merely tools of empire but multi-faceted products of the interaction between international, imperial and colonial forces.[14]
Colonial rule in some parts of Asia was brief; Nicholas Tarling has deemed it a ‘a fleeting, passing phase’ in Southeast Asia.[15] An exception is the Philippines, where a relatively short period of American colonialism was preceded by over three centuries of Spanish colonial rule. Thus scholars like Warwick Anderson can trace a history of racial policy and deferred citizenship during the American period, where policies became a way to mark Filipinos apart from Americans, yet also allowing some of the former to transition properly into the latter. In the perspective of many American hygienists, Filipinos were ‘half devil and half child’, possessing a contaminating body that could be put right by the efforts of American physicians and a small number of enlightened Filipino doctors.[16]
Anderson’s approach differs from Ken De Bevoise’s study of the origins of the major health crisis in the Philippines in the late-19th century during the final years of Spanish colonial rule. De Bevoise is no less critical about power and domination than Anderson, but dwells instead on an ecological account of epidemic disease. It is the long-term factors that have explanatory force here: the demographic, economic, social, technological, and political changes over the longue durée that affected and reshaped the relationship between humans, pathogens and the environment.[17]
Finally, there is the case of semi-colonial situations such as modern China in the 19th and 20th centuries. This is a useful extension of how colonialism was never complete or hegemonic. In Ruth Rogaski’s nuanced reading, the pursuit of hygiene was a major part of the difficult Chinese struggle for modernity. Colonial medicine in the micro-urban contexts of the treaty ports was not monolithic or all-conquering. It changed over time, involving collaboration between foreigners and locals.[18] The colonial period in China was also a relatively short interlude. Mary Augusta Brazelton’s survey of vaccination there after 1949 shows how, as a form of medical technology, it gave the Maoist state vast control not only over disease but also human bodies and lives. The outcome was not a suppressed population, as David Arnold and others have argued. There was popular support for vaccines that worked, so much so that they have come to define the meaning of Chinese citizenship.[19]
Another aspect of the Chinese literature is relevant to places like Singapore. The study of Maoist China reminds us that a history of pandemics needs to traverse into the post-colonial era. Colonial rule gave historians a substantial trove of archival documents that recorded not only the work of health departments and administrators, but also their perspectives, priorities and politics as colonial developers. It is more difficult to gain access to post-colonial archives in many Asian contexts. In Singapore, most government records after the British left are still classified, including those of the ministries responsible for health and disease.[20] This is likely true for many other Asian countries. Yet, it is paramount that creative efforts are made to locate other forms of local sources so that post-colonial histories can be attempted.
As much as the colonial era ought not to be seen in isolation from the longue durée and the ecology of epidemic disease, it similarly cannot be understood without reference to the period that followed it. Colonial medicine may have an impact on its successor through the international circuits of scientific collaboration and exchange that emerged with the end of colonialism. The question at hand is the balance of historical change and continuity. A post-colonial history of pandemics places colonial accounts in perspective, and vice-versa. There are pandemics that straddled both periods, such as those of influenza, cholera, poliomyelitis, and diphtheria. Of those that are contemporary, such as the coronavirus pandemics, their study may offer new insights on what happened in history. We can better understand both the past and present by venturing into the post-colonial era.
In conclusion, the lessons of history are not a ‘copy and paste’ from the past. The learning points we look to draw are more modest ones. We are able to consider alternative actions or new options, based on evidence and with the benefit of hindsight. Why Singapore did not respond sufficiently to influenza pandemics in the 20th century, for instance, is something we can contemplate. This does not tell us what to do in the next pandemic – that can only be decided by the leaders, the medical experts and the people, using all the facts at their disposal, including biomedical and historical facts. Drawing lessons from history is often difficult but important. It may raise more questions than answers and is likely to require scrutinising common myths and outlandish claims.
______________________________________________
[1] George Dehner, Global Flu and You: A History of Influenza (London: Reaktion Books, 2012).
[2] Mark Honigsbaum, The Pandemic Century: A History of Global Contagion from the Spanish Flu to Covid-19 (W.H. Allen, 2020).
[3] Catherine Arnold, Pandemic 1918: Eyewitness Accounts from the Greatest Medical Holocaust in Modern History (St Martin’s Press, 2018), p. 13.
[4] Niall Johnson, Britain and the 1918-19 Influenza Pandemic: A Dark Epilogue (London and New York: Routledge, 2006).
[5] Furtado, Plague, Pestilence and Pandemic, p. 12.
[6] Johnson, Britain and the 1918-19 Influenza Pandemic.
[7] Furtado, Plague, Pestilence and Pandemic, p. 12.
[8] Ed Yong, ‘How Did This Many Deaths Become Normal?’, The Atlantic, 8 March 2022, https://www.theatlantic.com/health/archive/2022/03/covid-us-death-rate/626972/
[9] David Arnold, Colonising the Body: State Medicine and Epidemic Disease in Nineteenth-Century India (Berkeley: University of California Press, 1993).
[10] Arnold, Colonising the Body.
[11] Kah Seng Loh and Li Yang Hsu, Tuberculosis – The Singapore Experience, 1867-2018: Disease, Society and the State (London and New York: Routledge, 2020).
[12] Lenore Manderson, Sickness and the State: Health and Illness in Colonial Malaya, 1870-1940 (New York: Cambridge University Press, 1996), p. 10.
[13] Giles-Vernick and Webb Jr., Global Health in Africa.
[14] Sandhya L. Polu, Infectious Disease in India, 1892-1940: Policy-Making and the Perception of Risk (New York, Palgrave Macmillan, 2012).
[15] Nicholas Tarling, Imperialism in Southeast Asia: ‘A Fleeting, Passing Phase’ (London; New York: Routledge, 2001).
[16] Warwick Anderson, Colonial Pathologies: American Tropical Medicine, Race, and Hygiene in the Philippines (Durham: Duke University Press, 2006), p. 4.
[17] Ken De Bevoise, Agents of Apocalypse: Epidemic Disease in the Colonial Philippines (Princeton: Princeton University Press, 1995).
[18] Ruth Rogaski, Hygienic Modernity: Meanings of Health and Disease in Treaty-Port China (Berkeley: University of California Press, 2004).
[19] Mary Augusta Brazelton, Mass Vaccination: Citizens’ Body and State Power in Modern China (Ithaca and London: Cornell University Press, 2019).
[20] Loh Kah Seng and Liew Kai Khiun (eds.), The Makers and Keepers of Singapore History (Singapore: Ethos Books and Singapore Heritage Society, 2010).
______________________________________________
* Banner image is an colonial account of the 1918 influenza pandemic in Singapore. Source: CO 275/101 Straits Settlements Medical Report 1918, p. 441.
* This article forms part of the research output of the Heritage Research Grant Project: Pandemics and Major Epidemics in Singapore, 1819-2021. The HRG Project is supported by Heritage Research Grant of the National Heritage Board, Singapore. Any opinions, findings, and conclusions or recommendations expressed in this chapter are those of the authors and do not necessarily reflect the views of the National Heritage Board, Singapore.
*The views expressed in the blog are those of the authors alone. They do not reflect the position of the Saw Swee Hock Southeast Asia Centre, nor that of the London School of Economics and Political Science.