Rising overmedicalisation of childbearing in low income countries is seen as a worrying trend as resources are scarce and could create a further risk for mother and child’s health. Here, Tiziana Leone summarises her recent paper which explores the driving forces behind the phenomenon in India.
Rising overmedicalisation of childbearing in low income countries is seen as a worrying trend as resources are scarce and could create a further risk for mother and child’s health. Here, Tiziana Leone summarises her recent paper which explores the driving forces behind the phenomenon in India.
Many low- and middle-income countries often struggle with persistently high levels of maternal mortality. This is coupled with rising levels of ‘overmedicalisation’, most commonly measured by rates of non-emergency caesarean delivery. Caesarean sections are used as an indicator of the level of quality of care given to women when giving birth but concerns around non-clinical reasons for performing the procedure are often ignored.
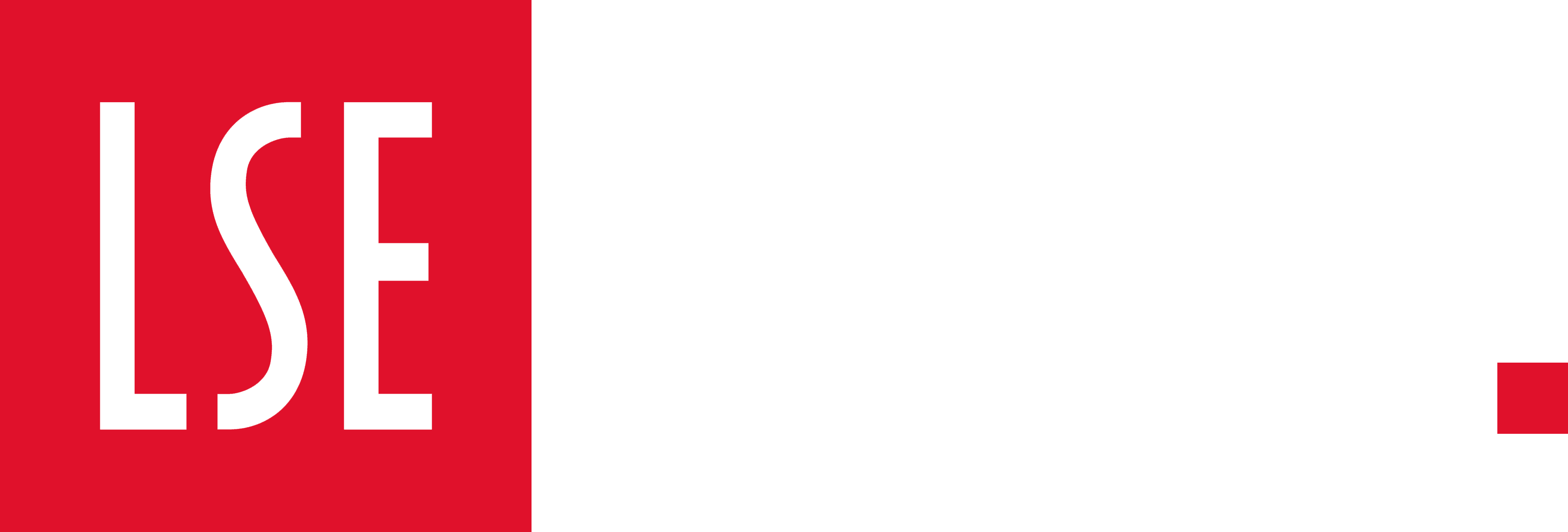
The World Health Organisation used to consider the minimum level of caesarean section rates to be 5% in order to be able to cope with emergency cases. The maximum was set to 15% and anything beyond this would be seen as overmedicalisation. For example, the UK C-section rate is currently around 23%, indicating a number of non-essential procedures are carried out each year. However, even higher levels of C-section are recorded in Latin America with Brazil reaching 40%. In some Indian states, such as Kerala, the rate is around 30%.
Little is known on the driving forces behind overmedicalisation of births. Advances in surgical techniques have made cesarean delivery much less risky, encouraging Indian obstetricians to perform more of them. Legal liability, heavy reliance on doctors for delivering rather than midwives and financial gains have also been accused of the increased levels of C-sections, along with patients fear of pain. Previous studies in South Asia have shown that overmedicalisation is not only detrimental for the wealth of the health systems but also for the push to increase institutional births as women become wary of delivering in hospitals. Ultimately an unnecessary C-section is a further risk for women’s health in low income settings, as well as a violation of her body.
Using national district level data from six Indian states (Punjab, Delhi, Maharashtra, Andhra Pradesh, Kerala and Tamil Nadu) I have analysed the risk of having a C-section controlling for socio-demographic factors such as maternal age, birthweight and wealth status. The states were chosen for their caesarean rates (at least 10% at state level), regional divide (north/south) and health systems’ features. Gender preference was also taken into account: Punjab, Delhi and Maharashtra tend to show a strong preference for male children, while Kerala, Tamil Nadu and Andhra Pradesh traditionally have a low gender preference.
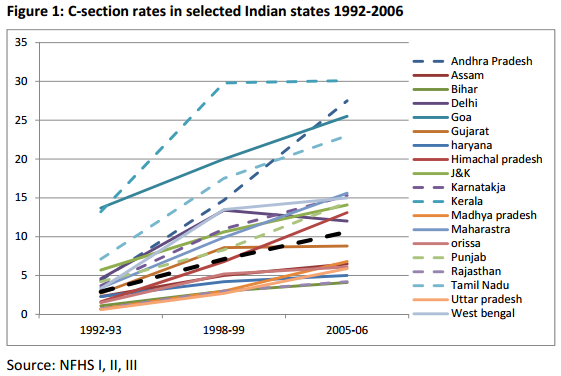
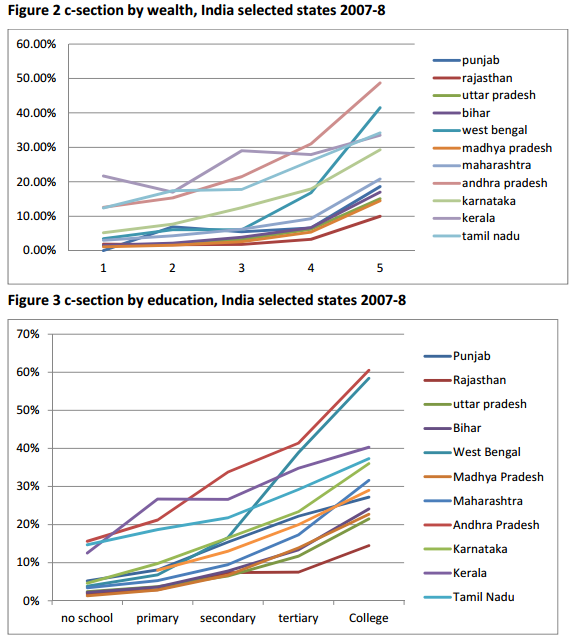
During the survey period there were 117,309 births across the six states. The analysis showed that cesareans were more likely at private than public institutions demonstrating a supply-driven phenomenon (see figure 1). In terms of demand, higher education levels rather than wealth seemed to increase the likelihood of a cesarean delivery (see Figs. 2 and 3).
Of note is that the data came just after the introduction of the Janani Suraksha Yojana (JSY) a cash transfer initiative aimed at increasing institutional births in India. The study showed that there are signs of the appropriate use of cesarean among women in the poorest strata, which might be due to initial progress made by the JSY program which has increased access to services for the poorest strata. However, this might also indicate a negative impact of the JSY program: because more money is paid for cesarean deliveries, hospitals’ motives might be driven by profit rather than by needs given that doctors are paid more and might be more willing to perform one when not needed. Significant district level results showed the influence of the health systems which is far stronger than community showing a further push from the supply side.
This study calls for more in-depth research into this phenomenon, a greater attention to pre and intrapartum protocols and a further push for greater involvement of midwives rather than doctors in safe deliveries. It also raises the question of whether the push for increased institutional deliveries in a country with a high maternal mortality could be compromised by a shift towards too much intervention.
This blog is based on Leone, Tiziana (2014) Demand and supply factors affecting the rising overmedicalization of birth in India International Journal of Gynecology and Obstetrics 127(2). Access the full article online here.
Note: This article gives the views of the author, and not the position of the India at LSE blog, nor of the London School of Economics. Please read our comments policy before posting.
About the Author
 Tiziana Leone is a lecturer in Demography in the Department of Social Policy at the London School of Economics.
Tiziana Leone is a lecturer in Demography in the Department of Social Policy at the London School of Economics.