Africa’s unprecedented growth in human population and urbanisation will likely exert more pressure on ecosystems, mainly through the transformation of food systems. These changes would heighten the risk of many infectious diseases, including those shared between humans and animals. Identifying sustainable food production systems in line with the One Health framework is therefore essential to pre-empt future pandemic, epidemic or endemic diseases.
This article is part of the series “Rethinking zoonoses, the environment and epidemics in Africa”, which examines the effect of changing relationships between human, animal and environmental health on epidemic risk.
Africa has the greatest infectious disease burden in the world, given its inadequate health delivery systems and under-investment in preventative services. This burden is expected to worsen as the continent’s human population, currently estimated at 1.39 billion, continues to rise. The continent currently has the highest annual growth rate globally of 2.5%, and the second highest population density of 45 persons/km2. Urbanisation is also rapidly increasing in the region; the proportion of the people who live in urban settlements is estimated to be 41%. Countries with the highest urban populations in the region include Gabon, Libya, Djibouti, South Africa and Nigeria.
A growing human population and rapid urbanisation increase infectious disease burden in many ways. They increase contact networks and the densities of susceptible hosts that amplify the transmission of disease-causing agents (such as bacteria, viruses and helminths); exert more pressure on available health care services, causing disparities in health service delivery; and drive environmental fragmentation and depletion following increased extraction of environmental services such as food, water and fuel to meet their ever-rising demand.
The latter pathway is usually associated with the transformation of food systems, which occurs as the demand for food heightens. Examples of food production enterprises that typically emerge include the intensification of livestock farming, the development or expansion of irrigation schemes to boost crop or fodder production, and deforestation to obtain more land for farming, among others.
Outbreaks of many infectious diseases, including those that are shared between humans and animals (called zoonoses), have been associated with food systems transformation. These diseases can be classified into three broad categories, depending on how they manifest. They may occur as (i) epidemics or pandemics, with explosive events that spread rapidly across populations and food supply chains, (ii) “silent” epidemics caused by infectious agents, such as antimicrobial resistant (AMR) bacteria or intoxications caused by drug- or pesticide residues in food, or (iii) smouldering infections that occur at a constant rate in populations, leading to high health and economic burdens.
Epidemics of zoonotic diseases such as bird flu or highly pathogenic avian influenza (HPAI), Rift Valley fever (RVF) and anthrax have occurred periodically in many food systems in Africa, with severe human health consequences. Recent HPAI epidemics were reported in commercial poultry farms in South Africa, Nigeria and Ghana. Similarly, a localised outbreak of RVF occurred in northern Kenya in 2021 in low-lying irrigated areas along the Ewaso Nyiro river, where crop irrigation farming was underway. Up to nine people succumbed to infections that they contracted during the outbreak. Many more infections and mortalities associated with food-borne pathogens, such as Escherichia coli and Campylobacter jejuni, have occurred in numerous areas. Children who survive such bacterial infections may suffer stunted physical and mental development, which limit them from attaining their full potential later in life.
The threat of “silent” epidemics is also enhanced by the application of more drugs at production units to enhance food production. Data on volumes of drugs that are being used in the region on an annual basis are scanty. Globally, however, up to 60,000 tons of antimicrobial agents are used to support livestock, aquaculture and crop production; about 90% of these usually end up in the environment. These products are likely to promote emergence and transmission of AMR, especially when excreted to the environment. The prevalence of AMR bacteria has been rising steadily especially in areas with intensive livestock and crop production systems. This menace threatens the effectiveness of drugs that are available for treating human and animal diseases, and would complicate the management of many infectious diseases and delay the attainment of most of the sustainable development goals.
Many of the control measures that have been employed to manage the health challenges illustrated above have failed to generate intended benefits because they have been one-sided, poorly targeted and inadequately resourced. Comprehensive, multisectoral and interdisciplinary approaches, founded on the One Health framework, are needed curb this challenge. One Health approaches, which acknowledge the interconnectedness between human, animal and environmental health, minimise negative externalities that are associated with food production, leading to sustainable and healthier ecosystems. They also improve efficiency of detection and response to zoonotic epidemics and pandemics mostly at the animal level and, hence, help pre-empt human exposure.
A similar principle on surveillance and response applies to the “silent” epidemics associated with AMR and other chemical agents and to mitigate the burden of so called “neglected”, endemic zoonoses. In addition, integrated surveillance to uncover health and development threats causing AMR and chemical residues consumed in food is urgently needed to increase awareness and hence action against this threat.
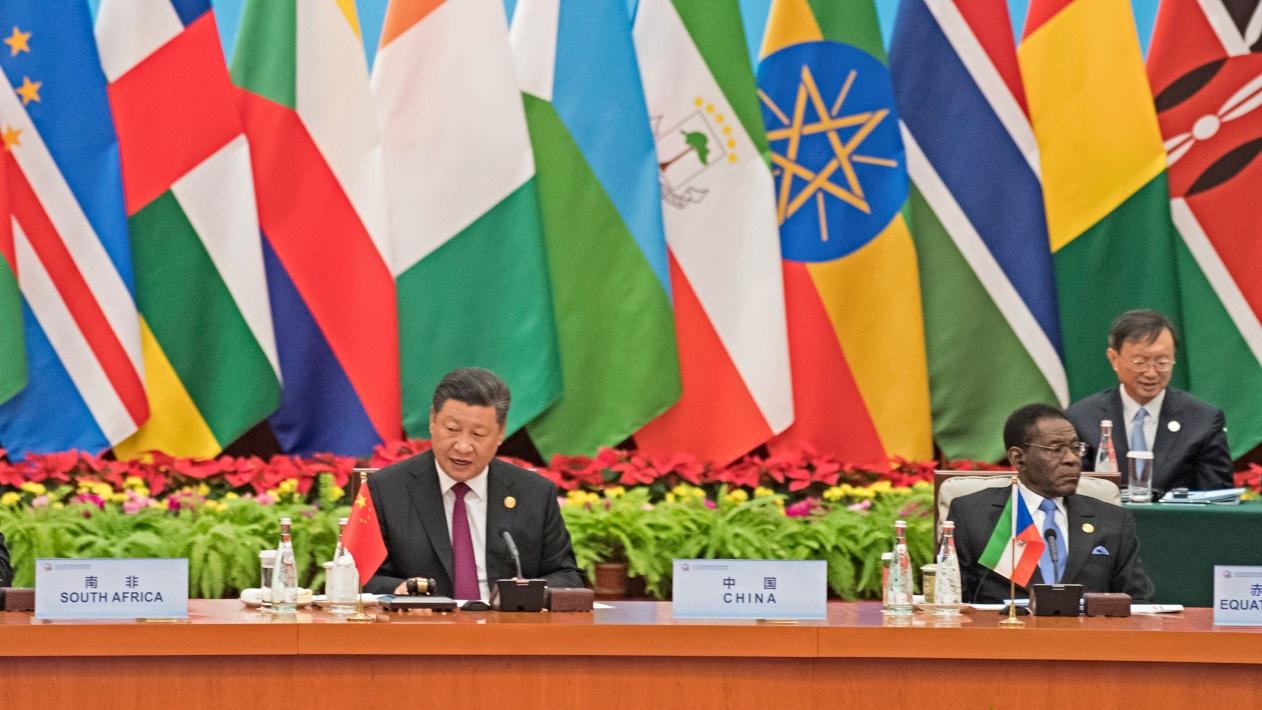
Featured photo: “Africa Food Security 11”. Stephen Morrison/Africa Practice. Licensed under CC BY 2.0.
Hero photo by RF._.studio from Pexels.




I don’t think there is any better way to put it!