Healthcare provision is vital for Africa’s wellbeing and economic development. Despite the challenges the continent faces in this regard, there are policy measures that governments can take that will ensure the health of their populations, writes Toluwalola Kasali.
Investing in healthcare is essential to developing human capital and a healthy young population that can contribute to the socio-economic development of a nation. Africa has a rapidly growing population of over 1.4 billion of which about 60 per cent are under the age of 25. The minds, expertise, ability, resourcefulness, creativity, and talent of Africa’s young population represent one of its greatest assets. However, the potential of this demographic dividend can only be fully realised through increased and sustained investment in their healthcare (physical and mental), skills, education, and overall well-being.
African governments need to invest in affordable and quality healthcare so that their populations can go to school, work, innovate, start businesses and be productive.
Governments in Africa, particularly Sub-Saharan Africa provide different levels of accessibility, affordability and quality of healthcare to their population, based on each country’s macroeconomic, political and social circumstances. However, some common policy challenges impede the provision of healthcare.
Governments should make strategic and sustained economic investments to strengthen their country’s healthcare system. In 2001, Member States of the African Union agreed to a target of allocating at least 15 per cent of annual budgets to improving the health sector. This is known as the Abuja Declaration. However, compliance has been uneven across the continent. Even in the face of budget constraints and competing spending needs, public health should be considered a priority for resources because of the knock-on benefits outlined above.
To help achieve this, governments can increase fiscal revenues by broadening the tax base. They could do this by introducing special levies or imposing taxes on unhealthy and harmful products and earmarking the revenues to finance public health services. The effectiveness of this approach will depend on the country’s tax administration capabilities including the ability to collect tax revenues and coordination with relevant ministries, including finance, health, trade, etc. To ease the political acceptability of new taxes, a phased approach can be considered to cushion the impact on the public.
Leadership and political will are vital to improving health outcomes and should be present at all levels of government. Countries facing macroeconomic challenges, weak currencies, and a high debt burden face tough decisions in funding development priorities. Therefore, political will and commitment to improving health outcomes will ensure continued support for the adequate financing of the health sector.
High out-of-pocket spending at the point of use of health services can create or worsen vulnerabilities and inequalities because they tie access to healthcare services to the level of citizens’ disposable income. Governments should develop efficient and effective health financing schemes like health insurance (national, social or community based), as they work towards universal health coverage to reduce dependence on out-of-pocket expenses. Policymakers can also consider integrating essential health services into social safety net programs, especially for vulnerable groups.
While a goal of many, progress towards achieving universal health coverage continues to vary by country. Policymakers often start with a set of benefits and the most vulnerable and gradually scale up by adding new benefits and new population segments. While progress continues to be uneven across countries, governments should accelerate the pace of coverage for all.
Having as universal as possible access to health helps to mitigate uncertainty and threats to public health systems from disease outbreaks, which can quickly spread across countries and populations. These can rapidly overwhelm weak health systems. Governments, therefore, need to proactively invest in research and support a resilient health system – one that can prevent, detect, and respond to public health emergencies while continuing to provide essential health services.
Primary healthcare is the foundation of universal healthcare, making essential and quality healthcare accessible and affordable to people, including physical, mental, and social care, particularly for women, children, and youths. For children, good nutrition is very important for their growth and development – especially in the first 1,000 days of their lives. A scalable, resourced, and integrated primary healthcare with an adequate referral system can reduce the burden on secondary and tertiary healthcare systems.
In many healthcare sectors across Africa, healthcare workers must deal with low wages, poor training, and underfunded facilities. In some African countries, this has increased strike actions and the migration of healthcare workers seeking better opportunities. Policymakers should prioritise better working conditions and salaries for staff. Policymakers should also consider how community-led services can be integrated into the healthcare systems, with training, financing, and infrastructure support.
The future
While there are many challenges, the future of health will look very different to how it is administered today. Digital health solutions can connect healthcare professionals to patients in real time and reach the unserved. To reap the benefits, policymakers must consider the local context and access needs, including mobile phone penetration, connectivity, and literacy.
A robust and effective health information system can safely and ethically provide integrated information that can be leveraged for evidence to make beneficial decisions for all stakeholders including patients, programs, and policymakers.
Such approaches will be vital as growing global insecurity and extreme weather have increased the need for emergency support. People fleeing their homes to safety or seeking relief from droughts, for example, have limited access to food, clean water, and good nutrition, which undermines their health and increases vulnerabilities to diseases. The impact of regional conflicts and climate change (drying waterways) can also affect trade and shipping routes which delay the availability of medical supplies and equipment. Policymakers should invest in local manufacturing capacities for essential medicines, vaccines, and other vital medical supplies. This will require partnerships between the public and private sectors.
The politics of health
Citizens pay taxes and, in exchange, expect quality and accessible public services, including healthcare. This social contract comes under daily scrutiny even more so in crises. Policymakers need to earn citizens’ trust by ensuring adequate public resources are allocated to healthcare fairly, timely and transparently with accountable systems and institutions.
Funding and programs for healthcare by governments, not-for-profit, and international donors are often fragmented and implemented in silos. Better coordination is required to reduce duplication, wastage, and inefficiency. Public financial management measures can also help to prioritise accountability, efficiency, and transparency to build trust with the public and meet fiduciary responsibilities to development partners.
Policymakers should consider incentivising or nudging people to make behavioural changes towards healthy and unharmful choices like choosing drinks with less sugar, reducing smoking, etc. which can contribute to improving health outcomes.
Investing in healthcare is essential to developing a healthy young population that can contribute to Africa’s socio-economic development – and policymakers will need to take action to realise the potential of this demographic dividend.
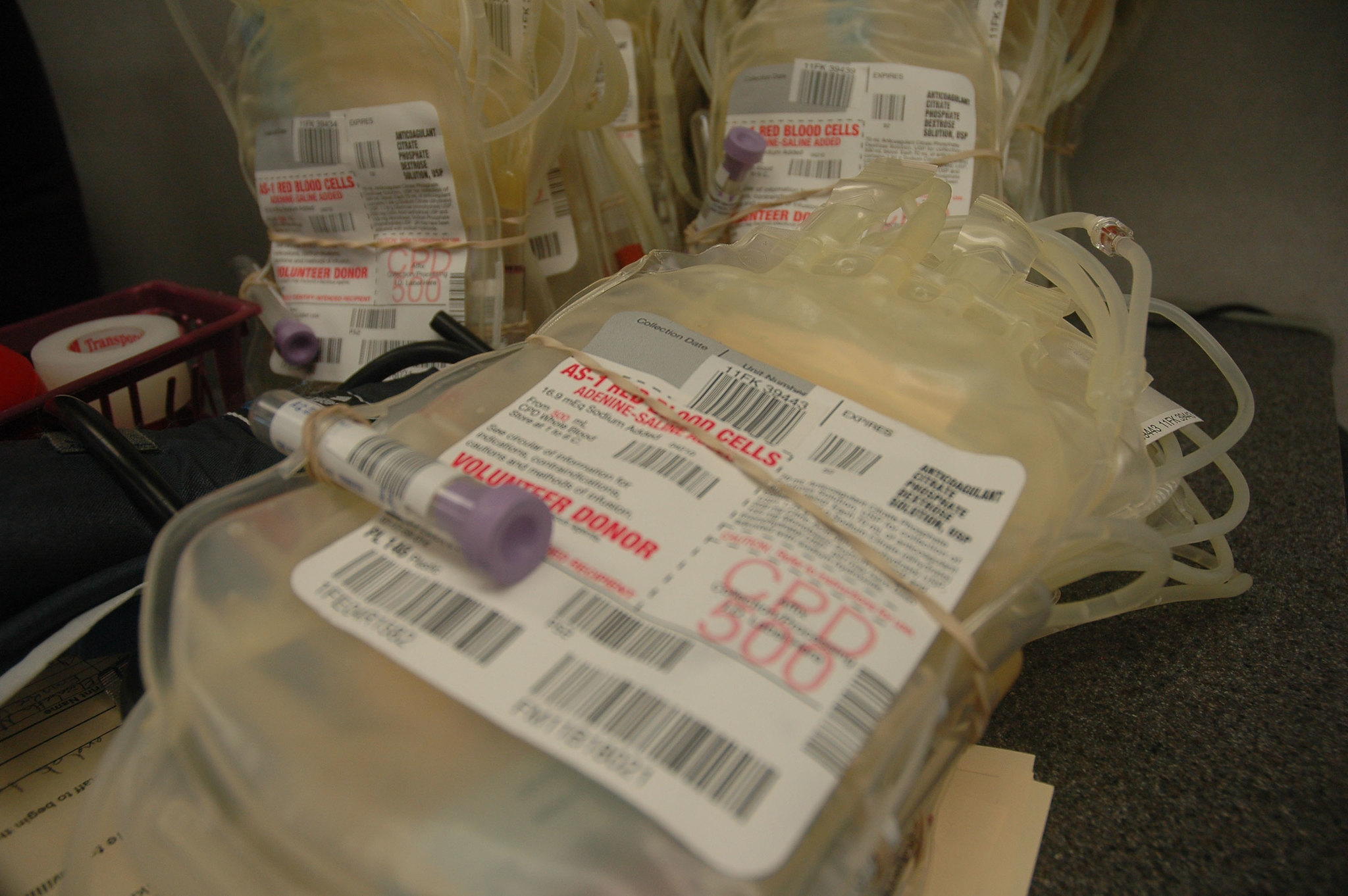
Photo credit: AMISON in the public domain.





Budget allocation is more challenging than ever in Sub-Saharan Africa, given numerous competing priorities, such as the escalating security threats. Additionally, improving health requires investment not only in healthcare but also in other determinants of health, including social, economic, and physical environments. A great article addressing a complex problem.