Although the ‘Spanish Flu’ killed almost a quarter of million Britons – many young – it went uncommemorated. Martin Bayly (LSE) explains how British society attempted to deal with the pandemic.
The sheer scale and devastation of the COVID-19 pandemic has brought renewed attention to the influenza outbreak of 1918-1919. Closer attention reveals both continuities and discontinuities between the two cases. Recent work by LSE academics focusing on the narration by policy elites of such ‘mass death’ events, and their societal impact, offers new interpretations of the 1918-1919 pandemic. In particular, this reveals the importance of commemorating the losses that are now being experienced once more.
The ‘Spanish Flu’ pandemic killed an estimated 228,000 in the UK, making 1918 the first year on record in which deaths exceeded births. (‘Spanish Flu’ was a misnomer. Spain’s neutrality within the war meant that its press was not subject to the same reporting restrictions and were among the first to report influenza cases, giving the impression it originated there.) In the US, an estimated death toll of 675,000 reduced the national life expectancy by 12 years. Elsewhere, the mortality rate was staggering. In South Africa, the relatively small population suffered a toll of 140,000 dead – mostly non-Europeans. Cape Town, it was said, was a ‘city of the dead’, with the Press Association reporting that some ‘native’ communities had been entirely wiped out. India suffered the worst toll, compounded by an ongoing famine, with estimates reaching as high as 18.5 million deaths. Globally more than one quarter of the world’s population contracted the virus.
The origins of the 1918 pandemic are contested, but one important vector was undoubtedly the movement of troops towards the latter stages of the First World War. Military bases in the USA that supplied troops for the American Expeditionary Force (AEF) as well as troop contingents in Northern France have been identified as one breakout site. More recent epidemiology suggests that the virus was in circulation in the two years immediately preceding the pandemic. The pandemic struck the UK in at least three discernible waves. The first, in the spring of 1918; the second, and most deadly, in the winter of 1918; and the third wave in the early spring of 1919. However, newspapers continued to report smaller outbreaks of influenza for at least another two years, and localised influenza outbreaks continued to be reported into the mid-1920s.
Although drawing historical parallels between then and now is tempting, there are important differences. A key contextual factor shaping the public and political response to the pandemic was the sheer uncertainty over what the disease was. Some senior medical practitioners and public health officials had experienced the earlier ‘Russian flu’ of 1889-1892. However few lessons seemed to have been learned in the interim; indeed, repeated influenza visitations arguably induced a degree of complacency. Virology remained in its infancy with medical science tending to the belief that influenza was a bacterium. This was significant since the smallpox epidemic of 1901-1904 had institutionalised a series of counter-measures for notifiable infectious diseases – including vaccination programmes. Influenza, however, was not a notifiable disease and vaccinations were not considered a worthwhile preventive measure, despite their use on military units. Added to this, 19th century ideas continued to shape thinking, with notions of the ‘miasma’, ‘bad air’, or ‘ill wind’ still prevalent in both received wisdom and official advice.
The First World War provides perhaps the central contextual factor shaping the official response. In material terms, there simply were not the resources for a comprehensive response. The war in Europe diverted medical practitioners away from the UK. Furthermore, the horrifying scale of fatalities as a result of the war had normalised death in such a way as to induce a degree of fatalism in the crisis narrative. Added to this, in the absence of comparative or time-series data, the public were given few tools to anticipate the future course of the outbreak, nor were policy elites willing to regularly narrate the chronology of deaths. The difference to today’s slick PowerPoint-led data-heavy government briefings is stark. Certain newspapers and public figures, including those within the medical profession, encouraged the idea that worrying about the disease would increase one’s susceptibility to illness and even weaken the nation’s resolve in the war effort. In the words of Sir Arthur Newsholme, the Chief Medical Officer of the Local Government Board (LGB), the national circumstances compelled an individual duty to ‘carry on’. The prevailing discourse behind the onset of the disease was therefore not one of a ‘war’ or ‘battle’, as with some of the rhetoric surrounding the response to COVID-19. Instead, the apparent viciousness of the influenza, and the speed at which it developed encouraged the language of an ‘attack’.
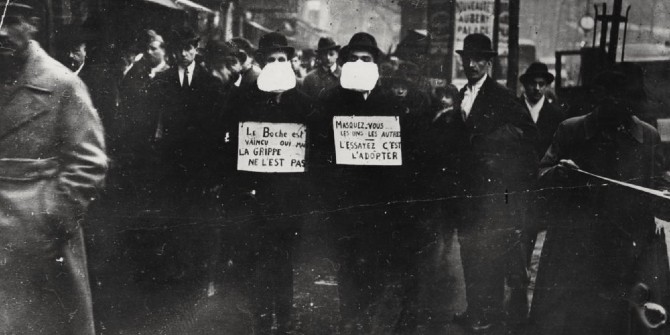
Despite the vectors appearing to come from troop movements, there was only occasional blame or responsibility accorded to soldiers. Unawareness of how the virus was spread meant attribution of blame tended to fall on a failure to observe proper sanitary habits. One frequent target of blame was the Local Government Board as the only organisation capable of oversight of the public health response by local authorities. Indeed, the absence of a nationwide public health body provides an additional distinction with the present crisis. In 1918 the Ministry of Health did not exist; it came into existence partly as a response to the pandemic in 1919. Public health was the responsibility of locally appointed Medical Officers of Health (MOHs), the Board of Education, and a number of ad-hoc bodies. This decentralisation of public health generated disaggregated and uneven countermeasures to address the outbreak. Whilst the proactive MOH at Manchester, James Niven, issued a public advisory as early as June 1918 and closed schools, this was far from standard practice. The LGB did not issue blanket advice till the advent of the second wave in February 1919, advising ‘healthy living’, well-ventilated rooms, warm clothing, and gargling with a solution of salt, warm water, and potassium permanganate. But few councils reproduced this systematically. Brandy and whiskey remained a popular remedy.
The vagaries of death reporting was an additional factor that shaped the public response. In the absence of a Health Ministry, death figures were collated and reported at the local and regional level – often through regional newspapers – and exhibited uneven practices. Influenza’s status as a non-notifiable disease further complicated recording of deaths. The comorbidities of pneumonia, bronchitis, heart disease, and phthisis (tuberculosis), were often reported in the death numbers alongside ‘influenza’, obscuring the deadliness of the virus. The absence of viral testing meant infection rates were not possible, whilst recovery rates were not reported. The virus proved disproportionately deadly to adults between the ages of 25-34, and women in particular. Whilst the gender ratios were overlooked, contemporary discourse privileged the deaths of the young, with the death of children understandably marked out as particularly tragic. Other communities also received disproportionate coverage and ‘heroisation’ including serving police officers, health workers, and soldiers.
The final area in which we can see lines of comparison relates to the practices of ‘death management’. As the LSE report demonstrates, the management of death, loss, and grief, and the commemoration or non-commemoration of these losses, carries with it the potential for long-term societal effects.
Funerals were not banned during the influenza pandemic, but body disposal was severely impacted by overworked undertakers, gravediggers, and coffin builders. Conscription led to a shortage in grave diggers and funeral workers. Even a shortage of horses and the low-quality feed available impacted on the provision of ambulances to remove the deceased. In Sunderland, for example, over 200 bodies were left unburied for over a week.
Crucially there is apparently no public memorial in the UK to the 1918-1919 influenza pandemic. This reflects international practice, with New Zealand providing one exception. The ambivalence of the state to influenza deaths despite the scale of loss added to the wartime context provides an explanation for the absence of public grief. The difference that public commemoration may have made to preparedness in later pandemics is a key counter-factual and arguably provides one of the most compelling ‘lessons’ from the 1918 pandemic.
Caution must be taken when comparing the present pandemic with the 1918 influenza outbreak in the UK. The wider context of the first world war and its aftermath was key in downplaying the crisis narrative. Rhetoric of a ‘war’ against the virus was absurd in this case. Scholarship has pointed to ‘war-weariness’ that seemed to shape the fatalism with which the outbreak was faced, but wider institutional, material, and social effects are apparent. The governing apparatus was radically different, and the paucity of virology expertise was decisive. The absence of an overarching health ministry created a disaggregated and uneven public health response. Rarely was the crisis grasped by governing elites, either rhetorically, or in practice. Even though funerals were permitted, the sheer pace of death fostered a silencing of grief. Less acknowledged in the literature is the fact that the devastation visited on troops was also silenced. Fighting men were permitted a hero’s death on the battlefield, but wartime restrictions meant reporting on the numbers killed by influenza was scarce.
Crucially, the second wave of the pandemic, which was more deadly than the first, appeared to generate more outspoken opinion against the response of the local and national government. In the medium term, newspapers remained alive to the possibility of later ‘waves’ of influenza for a number of years, demonstrating the long-tail impact of the pandemic on public awareness.
The way in which societies remember is not always a deliberative choice, but governments do have options. A failure to commemorate the 1918-19 pandemic silenced the deaths of hundreds of thousands of people, many of them disproportionately impacted by virtue of their gender or socio-economic status. The literature on war, memory, and post-conflict transition shows us that a failure to commemorate can hold long term implications for societal cohesion. But a failure to commemorate 1918-1919 also left the country ill-prepared to confront the next pandemic wave of 1957, and now the COVID-19 pandemic today. Memorialising the loss suffered as a result of COVID-19 should be a key area of government policy, for the good of society, and to ensure the hard-won lessons of this pandemic are not lost when the next one arrives.
This post represents the views of the author and not those of the COVID-19 blog, nor LSE. It is an edited extract from Confronting the COVID-19 Pandemic: Grief, Loss and Social Order (Department of International Relations, LSE).






Very informative article. Thank you.