 To accelerate robust growth and aspire to global power status, South Asian countries must improve their child health indicators. Drawing on her professional advocacy and communications experience in South Asia, Krupa Shah discusses the availability of preventative treatments for the most common infectious diseases and the barriers to achieving comprehensive immunisation programmes across South Asia.
To accelerate robust growth and aspire to global power status, South Asian countries must improve their child health indicators. Drawing on her professional advocacy and communications experience in South Asia, Krupa Shah discusses the availability of preventative treatments for the most common infectious diseases and the barriers to achieving comprehensive immunisation programmes across South Asia.
In 2015, just under 6 million children died globally, with more than 30 percent coming from South Asia. That is equivalent to eleven children dying every single minute worldwide. The consequences of these deaths shatter families and communities, and scar some of the world’s fastest growing economies.
This alarming rate of child mortality continues to happen despite the fact that some of these diseases are easily preventable. Although there are safe, proven and cost-effective interventions for key infectious disease such as pneumonia and diarrhea, they remain the leading causes of death. In South Asia, they account for 15 percent and 9 percent of all under-five deaths respectively.
The most common cause of diarrhea is rotavirus, which claims the lives of more than 200,000 children each year and is responsible for nearly 40 percent of all diarrhea hospitalisations. These conditions have long lasting negative consequences – for example, children often become more susceptible to other illnesses and have slower physical and cognitive development
Treatment options such as oral rehydration salts solutions and zinc for diarrhea and antibiotics for pneumonia are recommended to avert child deaths. However, though inexpensive and efficacious, the biggest constraint is the availability of these treatments in the areas that need it the most. Even when treatment is available, the high out-of-pocket expenses substantially burden the poorest of households. Although the saying ‘prevention is better than cure’ may seem clichéd, with infectious diseases, the preventive methods are already there, and it is imperative that we adopt them.
Immunising South Asia
Vaccines are the simplest and most cost effective tools to prevent infectious diseases. As seen with the introduction of vaccines, a recent study found a $16 return in healthcare costs and lost productivity due to care-seeking, death and disability on every $1 spent and a $44 return when we account for the value of people living longer and healthier lives in low and middle income countries.
More importantly, the introduction of immunisation in the recent years has had a dramatic impact in South Asian Countries. One of the most successful public health endeavors was an intensified polio immunisation campaign in India, home to half of all polio cases until 2009, which resulted in the complete eradication of the disease. Similarly, other South Asian countries such as Bangladesh, Bhutan, Maldives, Nepal, Sri Lanka have also been declared polio free. Additionally, through the introduction of Tetanus Toxoid (TT) vaccines, neonatal and maternal tetanus has been eliminated in many South Asian countries.

The most effective preventive measures that protect against pneumonia are two recent vaccines – Haemophilus influenzae type B (Hib) vaccines and pneumococcal conjugate vaccines (PCV). Moreover, there are oral rotavirus vaccines which would significantly reduce instances of diarrhea. However, the uptake and scale-up of these vaccines in South Asia has been remarkably slow and varied.
The PCV is a prime example of this mixed up-take. Through GAVI’s financial support, Pakistan was the first South Asian country to introduce PCV in 2012. Afghanistan, Nepal, Bangladesh and Myanmar have followed suit. However, India, a country that carries the highest burden of child pneumonia deaths globally, still has not introduced PCV into its national immunisation program.
Conversely in March 2016, India became one of the first South Asian countries to launch rotavirus vaccines in its national immunisation program. This will significantly help reduce the estimated 78,000 rotavirus-associated child deaths in the country. The vaccine was introduced initially in four states – Andhra Pradesh, Haryana, Himachal Pradesh and Odisha — and is expected be expanded to the entire country in phases. This is not only India’s first indigenous vaccine, but also the world’s cheapest vaccine at less than $1 a dose in a three dose regime for governments in low income countries.
However, there has been a slower rollout of rotavirus vaccines in the remaining South Asian countries. Earlier this year, Bangladesh and Pakistan submitted their GAVI application for the introduction of the rotavirus vaccines. Next month, the Punjab district in Pakistan will be the first to introduce the vaccine into its routine immunisation program. At this stage, other South Asian nation such as Afghanistan, Nepal, and Myanmar have no plans of introducing the vaccine into their national schedules until 2017 – 2020.
Barriers to implementation
While the solution is seemingly simple, there are many barriers to its implementation. A lack of political will has resulted in disproportionately small government healthcare budgets. The graph below shows public health expenditures reflecting % of GDP between 2000-2014 (source):
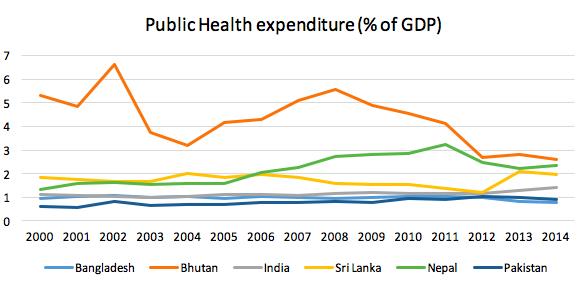
To put this into perspective – India spent 2.3% of its GDP on its military and was the world’s sixth largest military spender in 2015. However, even with the world’s highest child deaths, India’s public spending in healthcare stands at 1.4% of GDP in 2014, amongst the lowest in the world, as compared to 3% in China and 7.6% in the UK. As a result of skewed government priorities, thousands of children succumb to illness each day.
While activism and lobbying build pressure and generate two sided conversations in the west, it is often much less effective in South Asian countries. At a national level, advocacy has been loosely defined with no clear results that can be monitored or evaluated, apart from cajoling journalists and encouraging paid media. The media have a responsibility to mirror society’s needs, but as things stand accurate scientific and health reporting is undervalued. Better reporting could positively influence policy making and help the government define its health priorities, which in turn would allow colossal aid donations towards health policy advocacy to be redirected towards implementation efforts.
That said, the Indian government has taken several steps to rejuvenate the health sector. In December 2014, it launched an ambitious immunisation program, Mission Indradhanush, which aimed to achieve full coverage by 2020. In addition, it is promoting healthcare start-ups by launching initiatives such as ‘Start-up India, Stand-up India” as it recognises the potential for strong growth.
Moreover, many South Asian countries have experienced unprecedented growth in private healthcare spending within last decade. Challenging multinational pharmaceutical companies such as GSK and Merck, newer companies such as Bharat Biotech in India provide affordable life-saving vaccines. These companies offer promising opportunities for innovations in healthcare delivery, financing and manufacturing.
Conclusion
It is important to recognise progress to date. The under-five mortality rate fell by 59% since 1990 in the South Asia region. Cross-sector and public-private global health collaborations such as GAVI and tireless efforts of millions of front-line workers – vaccinators, social mobilisers and community and health workers – have been key in improving child health conditions. However, the child health inequities remain a severe threat.
During a discussion at the LSE last year, Amartya Sen invited us to recall, “the whole idea that you could somehow separate out the process of economic growth from the quality of the labour force is a mistake against which Adam Smith warned in 1776”. Similarly, to accelerate robust growth and aspire to become global economic powers, South Asian countries must improve its child health indicators.
It is our responsibility to give today’s children a better tomorrow. Universal immunisation will ensure each child a better chance of a fulfilling life. Together, this will make a healthier and more prosperous region.
This article gives the views of the author, and not the position of the South Asia @ LSE blog, nor of the London School of Economics. Please read our comments policy before posting.
About the Author
 Krupa Shah is pursuing an MSc in International Health Policy (Health Economics) at LSE. Prior to LSE, she worked with Deloitte Consulting in the healthcare space in New York, and recently spent 6 months working at an international health communications and advocacy organisation in New Delhi. Her interests include health financing, pharmaceutical economics and the role of the private sector in expanding healthcare access.
Krupa Shah is pursuing an MSc in International Health Policy (Health Economics) at LSE. Prior to LSE, she worked with Deloitte Consulting in the healthcare space in New York, and recently spent 6 months working at an international health communications and advocacy organisation in New Delhi. Her interests include health financing, pharmaceutical economics and the role of the private sector in expanding healthcare access.







Very well written. This article was super informative.
Thanks,
Preet