

 Providing care to an older adult spouse is an intensive activity that can substantially limit the employment opportunities and leisure time of caregivers, especially for those on low incomes. One way of providing them with needed support is through free access to health insurance. In new research, Joan Costa-Font, Nilesh Raut and Courtney H. Van Houtven find that the Medicaid extension as part of Patient Protection and Affordable Care Act (ACA), to all adults under 65 earning up to 138 percent of Federal Poverty Level, reduced caregivers’ depressive symptoms and improved their feelings of happiness.
Providing care to an older adult spouse is an intensive activity that can substantially limit the employment opportunities and leisure time of caregivers, especially for those on low incomes. One way of providing them with needed support is through free access to health insurance. In new research, Joan Costa-Font, Nilesh Raut and Courtney H. Van Houtven find that the Medicaid extension as part of Patient Protection and Affordable Care Act (ACA), to all adults under 65 earning up to 138 percent of Federal Poverty Level, reduced caregivers’ depressive symptoms and improved their feelings of happiness.
When informal caregivers in the US lack access to inexpensive health insurance, they may have to work longer hours to maintain their private health insurance plan, adding stress to their already hectic lives. This can have a detrimental effect on the mental health and general wellbeing of these unpaid caregivers, who would otherwise prefer to give up their jobs to take care of their loved ones.
In the United States, health insurance benefits have traditionally come from employment unless individuals qualify for public insurance (Medicare) at age 65, except for those on low incomes who can qualify for public insurance (Medicaid) throughout their working years and after. Limited employment opportunities might mean an increased the likelihood of not having any type of health insurance, increasing exposure to the health and financial hazards of poor health (including mental health), as health insurance is often linked to employment decisions. Limited health insurance can mean important negative consequences to the wellbeing of carers more generally, as it impacts the ability to engage in preventative activities (e.g., flu shots, preventive care, and screenings) and increases the stress associated with their daily duties.
Giving care to adult individuals makes it more likely they will fall into poverty, suffer losses at the height of their earning potential, and lose their health insurance without being eligible for Medicaid. This is particularly true for intense caregivers (those who provide 20 hours a week or more), who are forced to work fewer hours or quit their employment completely, which lowers their annual income.
It is estimated that 47 percent of caregivers who care for a disabled mother report having more depressive symptoms. Such effects emerge even when one looks at the rising use of gastrointestinal medications, tranquillizers, antidepressants, and painkillers.
How Medicaid expansion help informal caregivers
Medicaid expansion may help the informal family caregivers who are the backbone of the long term supports and services infrastructure. 19 percent of Americans are providing unpaid care to an adult with health or functional needs and 61 percent of family caregivers are employed. Family caregivers provide substantial cost savings to Medicare and Medicaid, but only a limited body of research has examined the effect of insurance expansions on spousal caregiver’s wellbeing.
Health insurance reform in the US, and more specifically the passage of associated Medicaid expansion law in 2010 (ACA Medicaid) gives us an opportunity to test the effect of Medicaid on caregivers’ wellbeing. Medicaid is the historic public insurance program that serves low-income US residents. From January 2014, several states expanded Medicaid eligibility criteria, as a part of Affordable Care Act (ACA), to all adults under the age of 65 earning up to 138 percent of Federal Poverty Level (FPL). The ACA Medicaid expansion significantly increased Medicaid enrolments and reduced the number of those without insurance, affecting the health, access to care, and health and care utilization for those gained access to health coverage.
Photo by National Cancer Institute on Unsplash
Health insurance, however, is just one of many obstacles that prevent caregivers from receiving the medical treatment they need; in comparison to non-caregivers, caregivers are known to struggle to obtain care for themselves or to put off receiving care. Therefore, the question of whether insurance expansion succeeded in raising the wellbeing of unpaid caregivers is one we can investigate.
Medicaid expansion made carers happier and less depressed
In new research, we find that Medicaid reduced the likelihood of depressive symptoms among spousal caregivers. We document that exposure to ACA Medicaid gives rise to an 8.2 percent points (on average, equivalent to 30 percent decrease) reduction in feelings of depression and 8.7 percent points increase in the feeling of happiness (on average, 11 percent increase). The estimates are robust to various specifications and are driven by reductions in out of-pocket expenses and labor supply and as expected, increased after Medicaid uptake.
Figure 1 shows that between 2012 and 2014 the ACA Medicaid expansion increased the feeling of happiness and decreased the feeling of depression for spousal caregivers living in expansion states, compared to their counterparts in non-expansion states. We observe that the parallel trends assumption appears to be satisfied for happiness and feeling depressed.
Figure 1 – Event study estimates—the effect of ACA Medicaid on happiness and depression
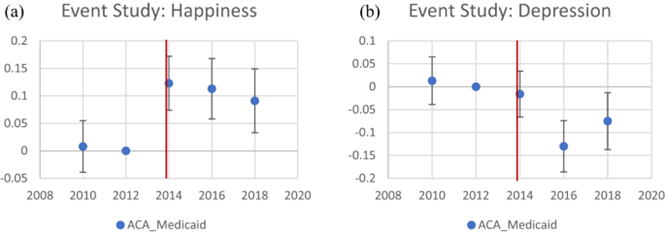
We also find an approximately 9 percent point increase in the feeling of happiness among spouses in the states adopting Medicaid expansion, compared to those in non-expanding states. Similarly, we estimate that the likelihood of feeling depressed decreases by more than 8 percent points after the ACA Medicaid reform.
The importance of supporting intensive informal caregivers
Our findings suggest that providing low-income adult spousal caregivers with health insurance can considerably lessen the psychological load of informal caregiving. Spousal caregivers gain from the ACA Medicaid program since it considerably improves their otherwise declining mental health.
We believe that supporting intensive informal caregivers is a key policy issue and a need of an hour because of following reasons: 1) Informal caregivers alleviate burden on formal health and care system. 2) Care provided by family member or spouse has significant impact on care recipients’ quality of life, promoting their emotional well-being. 3) Informal caregiving costs less than institutional care. Thus, it is cost-effective and can result in financial savings for families and governments. 4) Healthy caregivers can sustain the activity of caregiving for longer.
ACA Medicaid is thought to have improved the mental health of spousal caregivers by acting as an indirect caregiver support policy. To minimize the detrimental effects of caregiving on mental health while promoting the desire of older adults with disabilities to safely remain in their own homes, indirect and direct programs supporting the informal caregivers who serve as the country’s main providers of long-term care should be implemented.
- This article is based on the paper, ‘Medicaid Expansion and the Mental Health of Spousal Caregivers’ in the Review of Economics of the Household.
- Please read our comments policy before commenting.
- Note: This article gives the views of the author, and not the position of USAPP – American Politics and Policy, nor the London School of Economics.
- Shortened URL for this post: https://bit.ly/3QsOb4N






