Nicholas Barr (LSE) argues that the pursuit of herd immunity as a response to COVID-19 is profoundly mistaken. The error is no accident, but an example of a much wider class of error – mistaking a simple model (which can be useful to clarify thinking) for a good enough description of reality to be used as the basis for policy.
The inappropriate use of models is widespread, and leads to bad policy. The models implicated in the financial crisis are a graphic example. A more recent one is consideration of herd immunity as a way of tackling COVID-19.
A simple model of herd immunity
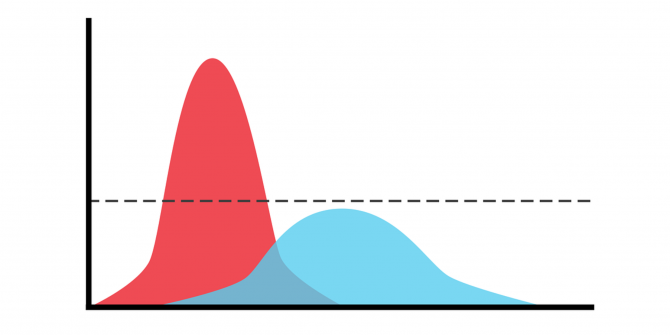
The idea, as explained more fully by my colleague Bob Hancké, is that once enough people have been exposed to the virus and have recovered (the example later in this article uses a figure of 75%), there are not enough non-immune people to allow the virus to spread.
The simple model of herd immunity works if:
a) Infection has a low mortality rate across all age groups (so that large-scale exposure causes few deaths);
b) Infection causes few or no long-term health problems;
c) A person who recovers has long-term immunity; and
d) The healthcare system has adequate capacity to address the full range of medical conditions.
In principle, this outcome can be achieved by speedy universal rollout of a vaccine that is highly effective across all age groups.
A slightly more advanced model relaxes assumption (a), so that there is an age gradient in mortality. In that case, the simple theory holds so long as
e) The at-risk group can be isolated in a way that is (i) effective and (ii) compatible with maintaining mental health.
Testing the assumptions

One has only to articulate these assumptions to see how far they deviate from reality.
a) There is overwhelming evidence of a steep age-gradient in mortality rates.
b) There is growing evidence that people in all age groups, and whether or not they have a pre-existing condition, suffer continuing health problems – so-called ‘long COVID’. Women in their 50s are thought to be at greatest risk.
c) The immune status of people who have been infected and recovered remains the subject of intense research.
d) In the UK last spring, the hospital system was severely stretched, and avoided being overwhelmed only by pausing large numbers of non-COVID-related investigations and procedures. The scale of the problem is illustrated by what are known as excess deaths, i.e. any excess in the number of deaths in a month relative to the long-run average in that month – widely regarded as the best single measure. Further evidence of extra non-COVID deaths is the recent evidence of a sharp increase in the numbers of people dying at home.
e) Shielding a large at-risk group faces multiple problems. First, protection is difficult even in a formal setting, shown by the large number of excess deaths in care homes earlier in the year, a problem that has not gone away. Second, many at-risk people live in multi-generation families – one has only to think of grandma in a family with a frontline worker who mixes with the public, and/or teenage grandchildren, who mix with their fellow students. Third, even where it is possible to isolate a vulnerable person effectively, the cost in terms of mental health is considerable for many people – that something is hard to quantify does not mean that it is not real and important. The problem of keeping in touch with relatives in care homes is well documented, exemplified by poignant pictures of people trying to talk through closed windows to elderly relatives, often suffering from dementia.
Finally, a vaccine that is highly effective, gives immunity for a significant time, and is available on a scale and at a price such that it can be rolled out rapidly universally at this stage remains a beguiling vision.
The moving parts: a numerical example
The table (spreadsheet available on request) illustrates a population of 1 million, a death rate of 1% and a target that 75% of the population should be survivors of infection.
It shows that in a simple setting with a 1% death rate, a policy of herd immunity leads to approaching half a million deaths (in the table, the number (highlighted in D10) is 488,722).
| A | B | C | D | E | |
|---|---|---|---|---|---|
| 1 | Number infected % | 50 | 75 | 75.188 | 100 |
| 2 | Absolute number infected | 500,000 | 750,000 | 751,880 | 1,000,000 |
| 3 | Number of deaths | 5,000 | 7,500 | 7,518.80 | 10,000 |
| 4 | Survivors of infection | 495,000 | 742,500 | 744,361.20 | 990,000 |
| 5 | Total surviving population | 995,000 | 992,500 | 992,481.20 | 990,000 |
| 6 | % immune survivors, living population | 49.75 | 74.81 | 75 | 100 |
| 7 | Immune, % of original population | 49.5 | 74.25 | 74.44 | 99 |
| 8 | Total deaths | ||||
| 9 | Deaths per million population | 7,500 | 7,518.8 | ||
| 10 | Deaths for UK population (65m) | 487,500 | 488,722 | ||
| 11 | Extra deaths (Goodhart effect) | ||||
| 12 | Extra deaths per million population (E3-D3) | 18.8 | |||
| 13 | Extra deaths for UK population (65m) | 1222 |
In Column C, 75% of the initial population (row 1), are infected, causing 750,000 infections and 7500 deaths (rows 2 and 3). Because of those deaths, survivors (row 4) are only 74.81% of the total surviving population (row 6), so that more people need to be infected to achieve the 75% target. Two effects are occurring, going in opposite directions:
(i) A death means that an infection does not result in an immune person, requiring an extra infected-and-then-immune person to fill the gap;
(ii) But, with a smaller population, fewer people in absolute terms need to be infected to reach the 75% ratio.
The effect of (i) is larger than (ii) because the target for herd immunity is not an extra immune person but 0.75 of an immune person, thus complete replacement for a death is not necessary.
The target of 75% infected-and-survived is achieved when 751,880 people have been infected (D2), with a total of 7518.8 deaths (D3), i.e. 18.8 people more than in the first pass in column C. Scaling to the UK population (assumed to be 65 million), the pursuit of herd immunity leads to 487,500 deaths in the first pass (C10) and a final total of 488,722 (D10), i.e. an additional 1,222 extra deaths (D13) because of the need to compensate for the deaths in the first pass. Those extra deaths are an example of Goodhart’s Law, explained by Bob Hancké.
What does this tell us?
The direct conclusion is that, even if the assumptions in the table hold, a 1% death rate leads to nearly half a million deaths. If 1% is on over-estimate, a death rate of half of that leads to nearly a quarter of a million deaths. However, the failure of the assumptions means that a death rate of 1% is sadly realistic; and even if the 75% target is achieved in the short run, without extended immunity, either natural or through a vaccine, any gains will be short-lived. Many people (definitely including Bob Hancké and me) regard the resulting deaths on anything like that scale as immoral.
The wider point is that it is a fundamental error to use a simple model in a complex setting. The simple herd immunity model is an epidemiological analogue of the simple model of a market economy (what economists refer to as a ‘first-best’ model), which assumes, for example, that all consumers are well-informed and have a long-run view, and that all firms and industries are perfectly competitive (the formal assumptions are set out in the Arrow-Debreu model).
The simple market model argues for consumer choice. But consumers of complex products are not well-informed, and mistaken choices may be deeply harmful. For precisely that reason the production and sale of pharmaceutical drugs are heavily regulated. The drive for that regulation was the string of deaths from patent medicines in the 18th and 19th centuries. We do not need to learn that lesson again. As my book on the welfare state explains, a central reason for substantial state involvement in cash benefits, health care and education in all developed and middle-income countries is as a response to market failure.
The simple herd immunity model, like the simple market model, is useful to assist clear thinking, but to use either as a basis for policy is an example of what I have called ‘pub economics’ – something that is obviously right, and everyone knows it’s right – but it’s wrong. In both cases, proponents make the mistake of believing that the simple model is the whole truth rather then – at best – an insight into part of the truth.
The fundamental error, in short, is believing that the model is a good-enough description of reality to work well in a policy setting. The error has two possible roots: either people genuinely believe that the model is an adequate description of reality, or their technical judgement is clouded by ideology.
Models should be used, not abused. As the economist and Nobel prizewinner Peter Diamond puts it:
‘The complexity of the economy calls for the use of multiple models that address different aspects. . . . I am concerned that . . . too many economists take the findings of individual studies literally as a basis for policy thinking, rather than drawing inferences from an individual study, and combining them with inferences from other studies that consider other aspects of a policy question, as well as with intuitions about aspects of policy that have not been formally modelled. Assumptions that are satisfactory for basic research, for clarifying an issue by isolating it from other effects, should not play a central role in policy recommendations if those assumptions do not apply to the world. To me, taking a model literally is not taking a model seriously. It is worth remembering that models are incomplete—indeed, that is what it means to be a model‘ (emphasis added).
This post represents the views of the author and not those of the COVID-19 blog, nor LSE. The author is grateful to Bob Hancké for helpful comments on an earlier draft, and for raising the subject in the first place, generating the email exchange that was the genesis of our twin articles.





A school boy error you have committed. People are heterogenous. The healthy have more interactions.
Immunity levels are at most 25% with reference to cities which have had no restrictions and prior immunity. London, NY, Brazilian ones.
It is also plain to see the London is pretty close to herd immunity. It has already worked.
Much better to ruin the lives of millions.
” Shielding a large at-risk group faces multiple problems. First, protection is difficult even in a formal setting, shown by the large number of excess deaths in care homes earlier in the year, a problem that has not gone away. Second, many at-risk people live in multi-generation families – one has only to think of grandma in a family with a frontline worker who mixes with the public, and/or teenage grandchildren, who mix with their fellow students. Third, even where it is possible to isolate a vulnerable person effectively, the cost in terms of mental health is considerable for many people – that something is hard to quantify does not mean that it is not real and important. The problem of keeping in touch with relatives in care homes is well documented, exemplified by poignant pictures of people trying to talk through closed windows to elderly relatives, often suffering from dementia”
How is this solved by lockdowns and restrictions?