What factors make for a successful vaccine rollout? Prashant Yadav (Center for Global Development/INSEAD) explains five of the key operational levers and choices that governments need to make.
Five key operational levers and choices determine how fast countries are able to roll out the COVID-19 vaccine. Ideally, someone at the national level makes these decisions, but this hasn’t always been easy in multi-level government systems.
1) Reducing supply variability at each level and prevent ‘over-buffering’
In some countries, clinics receive a very clear estimate about how many doses they will be sent each week for the next few weeks. In other countries, they only have opaque information to go on or only receive information about their next few days of supply, and this means they will hold on to vaccine doses because they’re worried about running out. Similarly, many clinics are reserving stock for the second dose because of uncertainty about future supplies. Better flow of information about supply and inventory across the different levels of government builds greater confidence in supply, and reduces “over-buffering”.
2) Scheduling, pre-registration and other ways to decrease demand variability

Appointment scheduling and registration systems are important levers to reduce the variability of demand at the vaccination clinic. Countries that had strong existing foundational layers of digital infrastructure have successfully built scheduling apps on top of such systems. Starting from scratch without a core underlying digital layer is more difficult, perhaps because of uptake and interoperability problems that occur when you roll out a new system in the midst of a pandemic.
3) Larger cohorts in each priority tier, and simultaneous start of more than one tier
With scarce supplies, prioritisation is important, but if the choice of priority tiers is such that the number of beneficiaries in each tier is large and the rules are simple – as in India (over-50s) or Israel (over-60s) – then the task of matching supply and demand becomes easier. The inevitable uncertainty over who comes to get vaccinated on a given day or in a given week at a given clinic becomes lower in larger tiers due to the statistical aggregation of uncertainty. Sequential prioritisation, in which priority groups are vaccinated in turn, is more likely to lead to supply and demand mismatching. If doses are left over, then the health workers have to allocate them hastily to people outside the tier, and that can create resentment among the general public.
This problem can be overcome by using simultaneous nested prioritisation. More than one tier is initiated for a vaccination at the same time but clinics keep a certain number of doses reserved for those in the higher priority tiers. This means fewer go to waste while prioritisation rules are still maintained.
4) Structure and design of distribution
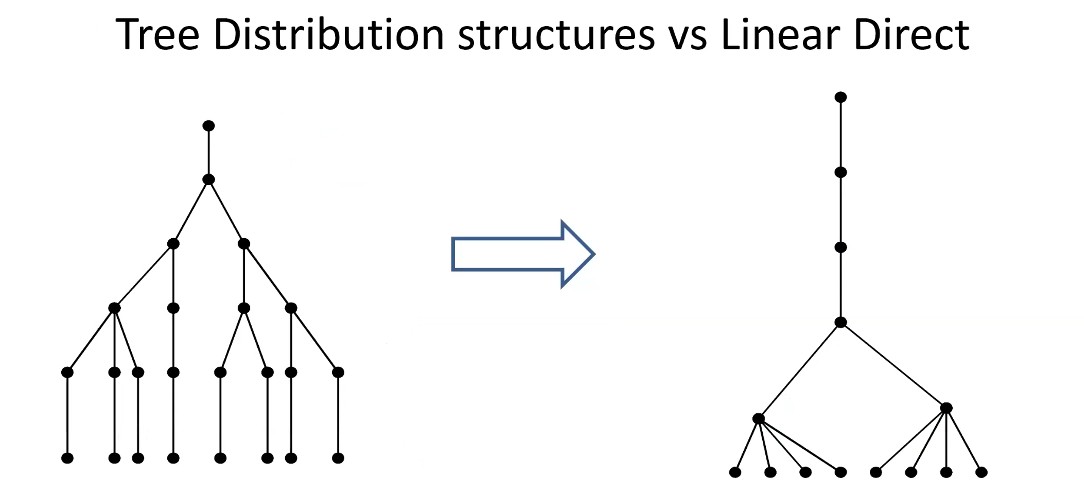
The conventional vaccination distribution system in many countries looks like an outward-branching tree. Some have now moved to a linear direct model for COVID-19 vaccines. That shift means new rules and new operating procedures have to be put in place, and has led to some initial glitches. But overall, a more direct distribution system helps in terms of information flow, better accountability and reduced needs for cold chain points, especially for vaccines requiring ultra-cold chain.
Another question that comes up is whether vaccination clinics/sites get doses based on the local population in their catchment area and the number of people in priority tiers, or should it depend on how many they have used in the past week? The answer to this is somewhat complex and depends on many behavioural factors. But in most cases, when the system has reached an equilibrium state, it will be possible to switch from a ‘push’ to ‘pull’ model where clinics request how many doses they want. But it is difficult to establish when a system has reached equilibrium state when there are multiple priority tiers and the rollout is sequential.
5) New mass vaccination sites, or existing sites only?
Should vaccination programmes use existing clinics and health facilities, as in India, or mass vaccination sites such as stadiums and sports arenas, as in the US and UK? Large sites increase throughput and pool demand in one location, so there is less uncertainty about demand and better ability to match demand and supply. Vaccination teams with scarce staff time are not waiting around and can make the best use of their time. The challenge for mass vaccination sites is operational design, as even small sub-optimalities in operational design get amplified and can create highly visible challenges when the a large number of people are coming to get vaccinated. Mass vaccination sites need to be very carefully planned and adequately staffed.
Even when thinking about its own vaccine deployment strategy, a country needs to remember that as long as the virus is not under control in all regions of the world the benefits will be short lived. The need for equitable global distribution also needs to feed into how we design the vaccination system. Governments may have to adopt a slightly more realistic expectation of the number of people they can vaccinate quickly when they take overall global access into consideration.
It goes without saying that increasing manufacturing capacity across all vaccine platforms, and making it sustainable, is crucial.
This post represents the views of the author and not those of the COVID-19 blog, nor LSE. It is based on Prashant Yadav’s contribution to How to Make COVID-19 Vaccination a Success, an event hosted by the LSE in January 2021.