What made a country less likely to record excess mortality during COVID? Research by Nikos Kapitsinis (Cardiff Business School) points to a strong test, trace and isolate system, well-funded healthcare, and earlier (but not longer) lockdowns.
Some countries have suffered much higher COVID mortality than others. In a paper for BMC Health Services Research, I look at the geography of excess mortality and its underlying factors in 2020, using regression analysis.
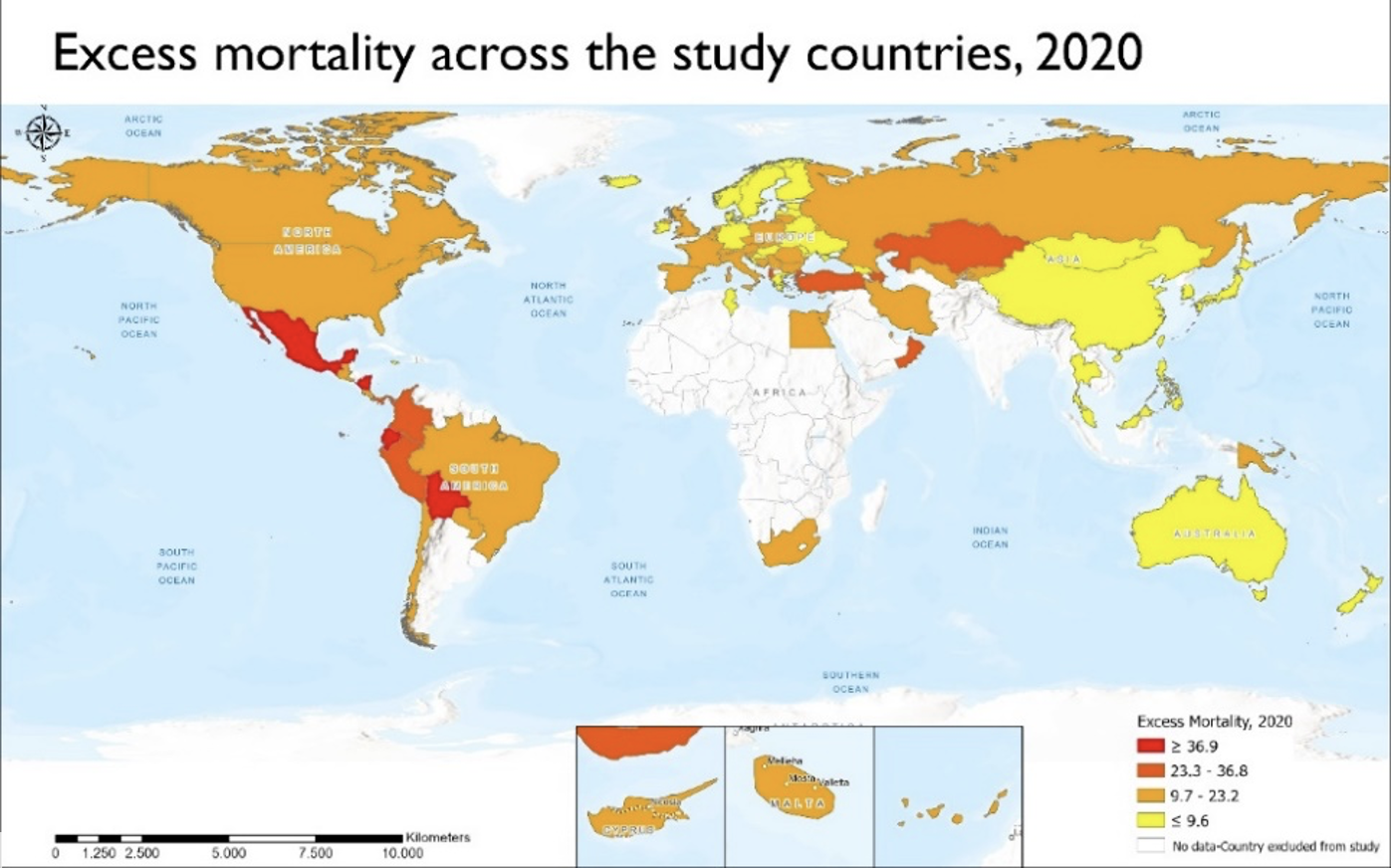
I estimated excess mortality in 2020 for 79 high, medium and low-income countries. Excess mortality in 2020 is calculated as the number of deaths in 2020 (as a percentage) compared to the average mortality from 2015 to 2019. Excess mortality captures the COVID deaths officially reported, COVID fatalities that were not registered as such, but also deaths that occurred due to other diseases that might have been prevented if the pandemic had not overwhelmed healthcare systems.
Around 3.7 million more deaths were reported in the 79 study countries in 2020 compared to the average fatalities between 2015 and 2019 — excess mortality of 13%. The study countries recorded more than twice as many excess deaths in 2020 compared to the officially registered COVID fatalities (3.7 million compared to 1.5 million), underlining the under-reporting of COVID deaths.
Figure 1: Excess mortality across the study countries
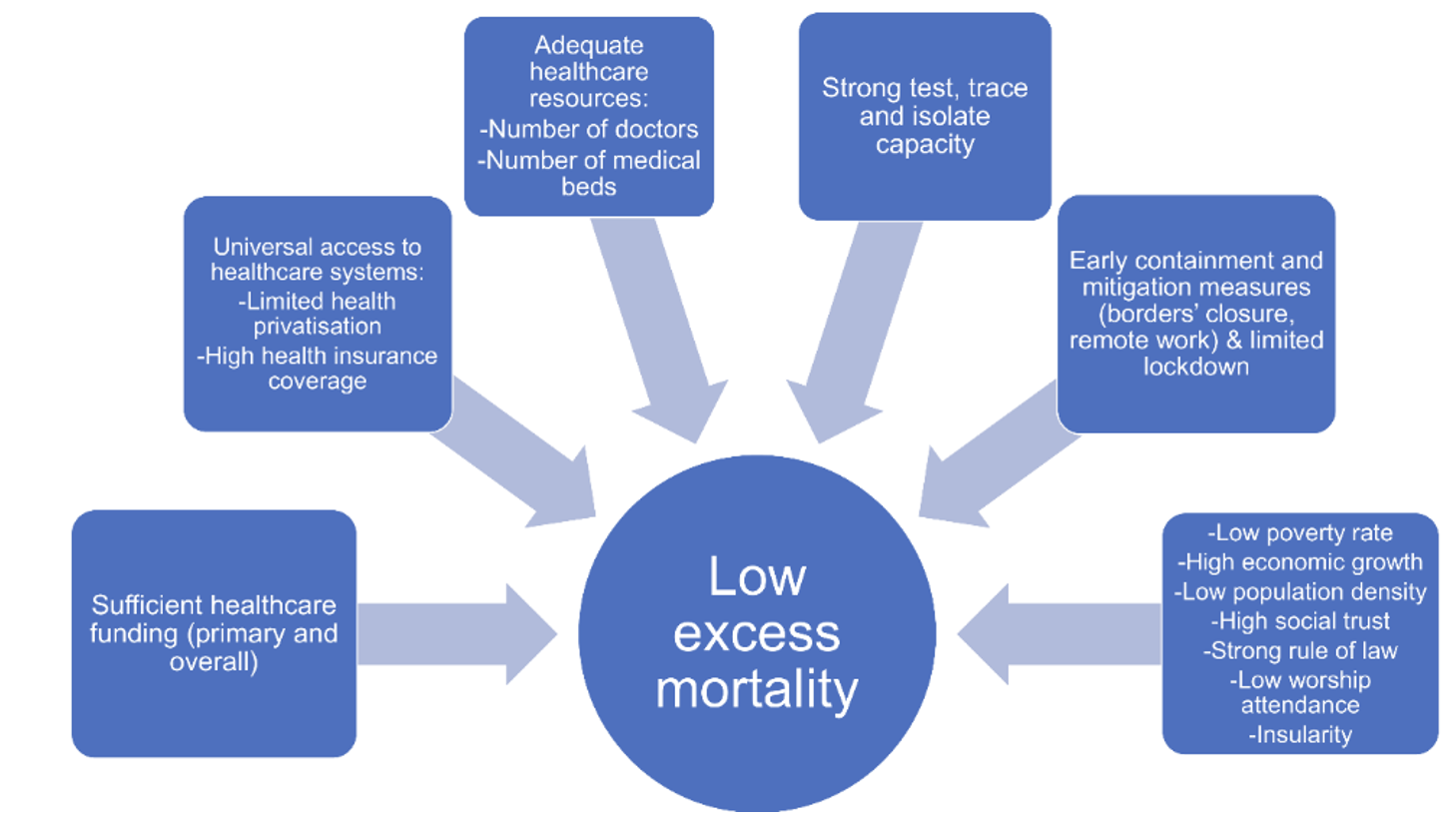
Better-funded healthcare systems were less likely to be overwhelmed. They responded more effectively to the pandemic and led to lower excess mortality. Moreover, countries with adequately-funded primary healthcare were more likely to record lower excess mortality, since COVID patients could be closely monitored at home to prevent their health deteriorating. This minimised the risk that healthcare workers and non-COVID hospital patients would contract the virus, and allowed hospitals to treat both seriously ill COVID patients and those suffering from other diseases.
Countries with extensively privatised health services (measured by the index of private health expenditure as a percentage of current health expenditure) saw higher excess mortality. Those that increased per capita health spending between 2008-18, on the other hand, were more likely to record low excess mortality. Services that were weakened by spending cuts during the austerity era struggled. The higher the share of the population covered by health insurance, and the greater the number of doctors and medical beds per 100,000 people, the less likely a country was to record excess mortality.

However, without effective government strategies even relatively strong healthcare systems could be overwhelmed. The average index of test, trace and isolate (TTI) proved to be possibly the most important determinant of excess mortality. Countries with a strong TTI capacity, such as Taiwan, were likely to have low excess mortality, probably because it enabled them to monitor the spread of the virus to inform policies. Targeted testing focusing on workplaces, care homes and schools is key to effective epidemiological surveillance. The estimated association between the number of COVID tests carried out per 100,000 people and excess mortality, however, was not statistically significant.
Countries that locked down their populations longest were likely to record high excess mortality
Contrary to mainstream policy narratives and beliefs, the countries that locked down their populations longest were likely to record high excess mortality. These countries often locked down too late and implemented delayed horizontal lockdowns that ultimately proved to be ineffective as they were not accompanied by intensive TTI. Countries which acted early showed lower excess mortality. Alongside TTI and international travel restrictions, the extended implementation of COVID safety measures at work (measured as the total number of days that any measure affecting the workplace applies) was also linked to low excess mortality.
The poverty rate proved to be a powerful driver of excess mortality. It often restricts access to healthcare, leads to poor living conditions and limits the capacity to physically distance. The infection rate is higher among people in lower social classes, who are forced to use public transport, work from home or live off their savings during lockdown.
Weekly worship attendance is associated with higher mortality
Densely populated and globally interconnected countries were more likely to record high excess mortality, as they struggled to identify travellers with COVID.
Countries with a high value on the rule of law index did better, since the effective implementation of emergency policies could facilitate a country’s response to the pandemic. Societies with fragile social trust were likely to demonstrate high excess mortality, since it weakens collectivism and social solidarity. Secular societies were likely to demonstrate low excess mortality: weekly worship attendance is associated with higher mortality. Several religious leaders have disputed the severity of the pandemic and expressed scepticism about the existence of COVID.
Figure 2: Factors in low excess mortality
Most states failed to cope well with the pandemic because they underestimated the severity of the virus, prioritising economic order. Their response was not timely, neglected TTI strategies and did not sufficiently support the healthcare systems, pinning all their hopes on vaccines. The spread of the Delta variant meant these vaccines ended up being less effective than promoted, and were in many cases used punitively to suspend healthcare workers. A lockdown can work if it is implemented early enough in places with a low infection rate, allowing governments to improve TTI capacity and provide the healthcare system with extra staff and equipment — potentially drawing on the private sector to do so.
This post represents the views of the author and not those of the COVID-19 blog, nor LSE.