Across the three waves of the Covid-19 pandemic that hit European countries in the space of twelve months, outcome indicators for Covid-19 cases and deaths diverged, as did policy responses. Linda Hantrais and Susanne MacGregor examine evidence about what societies and their institutions could have learnt from each other and from their own experiences during successive waves of the pandemic. They ask whether policy learning seemed to be more effective in some societies than in others, and if so why.
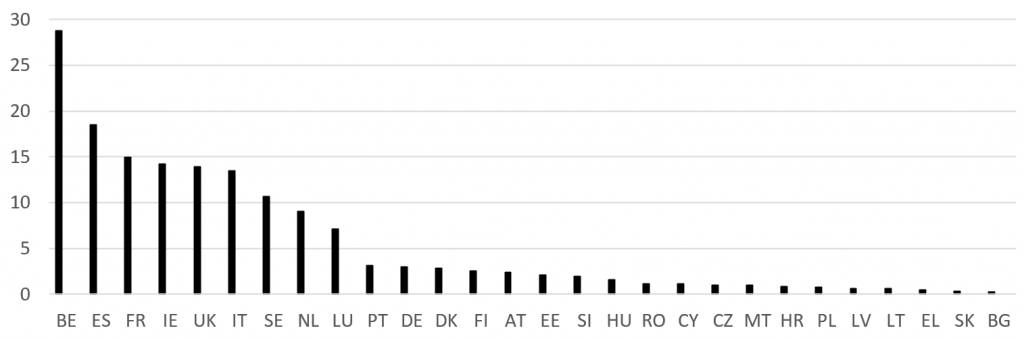
Between March 2020 and February 2021, the numbers of Covid-19 cases and deaths in EU member states peaked three times. The World Health Organisation identified Europe as the epicentre of the first wave in March 2020, based on the extremely high numbers of deaths recorded in several of the most densely populated countries (Belgium, France, Italy, Spain and the UK), whereas the Central and East European countries and small island states, which had joined the EU in 2004, remained almost unscathed (Figure 1).
Figure 1: Daily death rate peaks per million inhabitants in the first wave of the Covid-19 pandemic (2−25 April 2020)
Note: The figures are rolling seven-day averages in the EU27 member states and the UK. Limited testing and disparities in attributing the cause of death mean that the number of confirmed deaths may not accurately record the true number of Covid-19 deaths. Source: Our World in Data
The European Commission struggled to exert authority over its 27 member states within the limits of its legal public health competences for coordinating policy responses, while EU member states exercised their responsibility for defining, organising and delivering health services and medical care. Guided to varying degrees by the ‘best scientific evidence’ produced by international teams of experts, and in the absence of a collective EU-wide strategy, member state governments sought unilaterally to procure personal protective equipment and ventilators from third countries. Initially, with different speeds and degrees of stringency, they reacted by introducing travel bans, states of emergency and a plethora of restrictive measures, culminating in full social and economic lockdown.
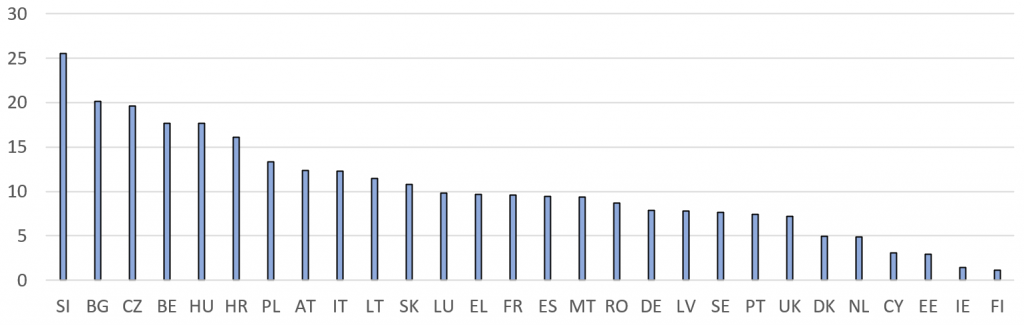
By the early summer, as predicted by the scientists, the epicentre shifted away from Europe to the Americas and southern hemisphere. Restrictions were progressively lifted, and a semblance of normality was restored, only to be followed, also predictably according to the scientists, by a second wave of the pandemic in the autumn (Figure 2).
Figure 2: Daily death rate peaks per million inhabitants in the second wave of the Covid-19 pandemic (5 November−21 December 2020)
Note: The figures are rolling seven-day averages in the EU27 member states and the UK. Source: Our World in Data
By late October, some of the same countries continued to display among the highest (Belgium) or lowest (Finland, Estonia, Cyprus) death rates, whereas others that had been largely spared in the first wave (Slovenia, Bulgaria, Czechia, Hungary, Croatia and Poland) saw death rates soar, making it difficult to ascertain whether any policy lessons had been learnt from their own experience or that of other member states.
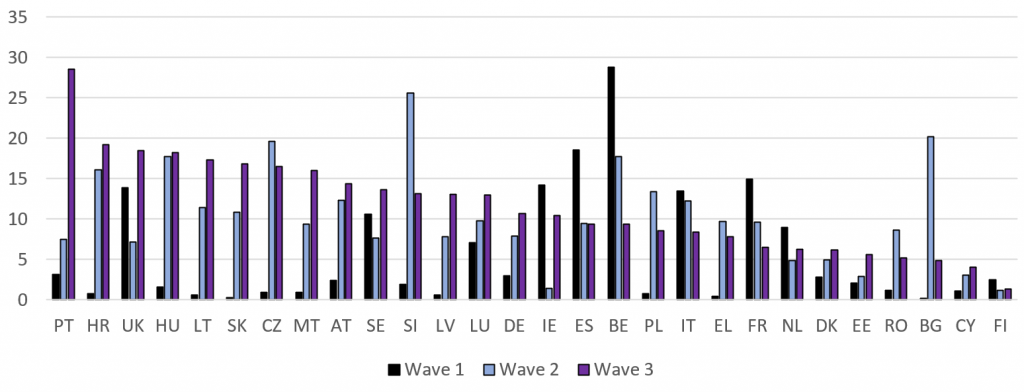
As autumn changed to winter, and governments across the EU reacted to domestic pressures to relax restrictions in the run-up to Christmas, temporarily allowing gatherings in family bubbles, a new surge – a third wave − in rates of infection and deaths was reported in late December and through January 2021. Even as effective vaccines were being approved and made available, new more transmissible strains of the virus sent hospital admissions and death rates spiralling out of control (Figure 3).
Figure 3: Daily death rate peaks per million inhabitants in the three waves of the Covid-19 pandemic
Note: The figures are rolling seven-day averages in the EU27 member states and the UK. The third wave is defined as 25 December-1 February 2021. Source: Our World in Data
National governments again responded unilaterally and differentially by restricting entry through their borders and reintroducing various lockdown measures. But, in the majority of EU member states and the UK, they failed to prevent third-wave peaks reaching higher levels than during the first and second waves of the pandemic. Only Finland, which consistently maintained the lowest death rates, and France, Italy, Belgium and Spain, which had previously reached some of the highest peaks, appeared to have fared better in the third than in the first wave of the pandemic.
The situation was further complicated when EU member states agreed to task the European Commission with negotiating block orders of vaccines on their behalf to avoid intra-European competition, only later to accuse the Commission of delaying and mishandling the procurement and rollout of vaccinations supplies, thereby exacerbating the tensions that had surfaced earlier in the year due to the sharing of competences for public health.
Opportunities for policy learning and transfer
The implementation of public health policies to deal with pandemics was known to be complex, making coordination and partnership critical; it requires a strong central state response, combined with active local involvement and good communication between different levels of governance and with the public at large.
In early 2020, much of the public discussion about the Covid-19 pandemic focused on the post-World War I ‘Spanish flu’, rather than other historical evidence. Common characteristics of previous epidemics were their sudden emergence, the initial absence of effective treatments or cures, a high burden of illness and death, and gradual awareness of long-term effects such as disability and socio-economic and health inequalities. Evidence from recent epidemics, especially SARS, demonstrated that the wearing of appropriate face coverings, physical distancing, hand hygiene and good ventilation are effective, relatively low cost, public health measures for containing the spread of the virus.
Past experience also teaches us the importance of global preparedness and adequate public spending; the need for infrastructures of surveillance and isolation, and for rapid outbreak response; the value of the standard public health strategy of contact tracing; the requirement for surge capacity in hospitals and healthcare services, and the need for both national and community involvement and for coordinated international responses. A further common feature identified in studies of pandemics by historians of public health has been the moralising or politicising of debate, and the role played by stigma.
Unlike earlier pandemics, during the first wave of the Covid-19 pandemic, scientists reported that older people and some other adults with co-morbidities and disabilities were more likely to experience severe symptoms and die from the disease. They predicted that infection and death rates would rise in cold weather when the public gathered in poorly ventilated spaces or were confined in crowded living conditions.
The European Commission and EU member states, especially countries that had been hardest hit during the first wave, might have been expected to use the knowledge gained from their own experience and from recent epidemics to avoid the worst effects of the continuing Covid-19 pandemic. They might have been expected to use the summer months to draw and apply policy lessons, not only from their own experience, but also from comparing and contrasting inputs and outcomes across European countries, to improve data collection and reporting procedures, to extend their understanding of the aetiology of the virus, to prepare more effectively for the second and subsequent waves of the pandemic, and to bring the disease under control.
Why were policy lessons not applied more effectively?
Despite the best efforts of analysts to establish linkages between outcomes and the stringency and timeliness of policy measures, the relationship between policies and outcomes, as measured by death rates, remained unclear. In the early phases of the Covid-19 pandemic, proponents of competing approaches suggested that countries such as Sweden and Germany could serve as models of disease control. As time went on, however, it became clear that no simple quick fix or one-size-fits all solutions would be found.
The overall picture after a year’s experience of Covid-19 in Europe revealed the limits of policy learning and transfer between member states. Social scientists have drawn attention to the socio-demographic, cultural, psychological, epidemiological, economic, legal and political determinants of public health within different societal contexts. Demographers and social policy analysts have shown, for example, that the odds were stacked more heavily against densely populated, internationally connected populations, with high old-age dependency ratios and high rates of underlying health conditions. Other determining socio-demographic, economic and environmental factors have been identified including high urban concentrations, poorly funded and equipped public healthcare provision, and underdeveloped technological infrastructures. Ethnicity, crowded living conditions and precarious working arrangements compounded the risk of contracting and dying from the virus once it became established in a population.
These effects might have been mitigated to some extent by efficient management of public healthcare resources, and adequate provision of preventative and protective measures for vulnerable population groups. Few EU member states were economically, physically, or politically equipped to meet fully the challenges of a pandemic. Rather, problems in dealing with Covid-19 were found to be amplified in situations characterised by entrenched political divisions, unstable or dysfunctional governments and sceptical electorates. More efficacious responses were determined to a considerable degree by political stability and consensus, public trust in governments and in the scientific evidence on which they relied as a basis for policy choices, a sense of individual and social responsibility and respect for the rule of law.
In different combinations, the multiple factors outlined above go some way to explaining the high rates of Covid-19 deaths in Belgium, France, Italy, Spain and the UK during the first wave, and why many Central and Eastern European countries and Portugal that were hardest hit in the second and third waves were unable to avoid its worst impacts through policy learning and transfer. Contextual information helps to explain why Germany was at an advantage in responding to the first wave of the pandemic, but not why the Central and Eastern European member states experienced very few Covid-19-related deaths at that time.
This analysis has highlighted the constraints on policy learning and transfer in the midst of a crisis. Accounts of the effectiveness, or otherwise, of national governments and the European Commission in implementing scientific advice need to take account of the great diversity between and within countries if they are to understand variations in the public health impacts of Covid-19 and state responses. While these complexities may help to explain why some countries seemed better able to respond to evidence and experience, only time will tell how thoroughly lessons were learnt.
Note: This article gives the views of the authors, not the position of EUROPP – European Politics and Policy or the London School of Economics. Featured image credit: Hospital CLÍNIC (CC BY-ND 2.0)