 Given that older people are an increasing share of society and that other pandemics will come, countries should revisit their priorities, writes Joan Costa-Font.
Given that older people are an increasing share of society and that other pandemics will come, countries should revisit their priorities, writes Joan Costa-Font.
The Covid-19 pandemic has hit the older population more than other age cohorts, as their weaker immune system makes it harder to fight diseases and infection. Although all age groups are at risk of contracting the virus, older people face significant risk of developing a severe illness. Of all coronavirus-related deaths so far, 95% occurred in those older than 60 years. More than 50% of all fatalities involved people aged 80 years or older.
Yet, not only older people are more exposed to the risk of contagion and death, but policy reactions have unveiled (i) the different social value older people have in different countries, (ii) the consequences of limited investment in quality long-term care across countries (in a context where nursing homes in many countries have become ‘death homes’), and (iii) the lower priority that older people have in congested health care systems. The question that remains open is then how to keep elderly people safer, and what to do if they do become infected with Covid-19, which I discuss at the end of the article.
The lower social value of the elderly costs lives
Covid-19 brings about key trade-offs: shutting down economic activity and restricting people’s freedoms, in exchange for improvements in wellbeing that encompass reduced fatalities, mainly among the older population. However, the social value or status of older individuals vis-à-vis other age groups in society is often overlooked in many policy responses.
Figure 1 – People over 70 are viewed with respect
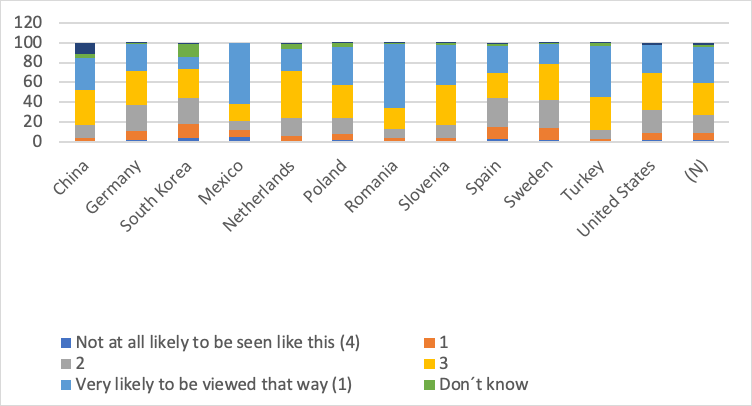
Source: World Value Survey 2010-14
Although with the ageing of the population older individuals certainly exert more political influence, their social value (or ‘social standing’ compared to other age groups) is very different across societies. Whilst many Asian countries report more positive perceptions towards older people, in many Western societies we observe a certain level of ‘age aversion’, where individuals praise youth stereotypes, and older people pretend to be younger to avoid the effects of ageism (or age discrimination). This can explain the late reactions to the virus, as noted by the World Health Organization’s director general, Dr. Tedros Adhanom Ghebreyesus, who accused some countries of seeing “old people as ‘less worthy’ of the best efforts to contain the virus”. But more generally, both in social media and in the press, we have seen an increase in discriminatory attitudes towards the elderly in these past few months (e.g., “They’re on their way out anyway”).
Cross-country survey evidence depicted in Figure 1 reveals how much respect people over 70 are viewed with in different countries (ranging from ‘not at all’ to ‘very likely to be viewed with respect’). As expected, in many Western countries such as Sweden, Spain, the US, the Netherlands, and Germany, people over 70 received a lower standing relative to other countries, whilst the opposite is true in Romania, China, Mexico, and Turkey. Differences in social perceptions underpin the social environment in European countries where we have observed delays in policy interventions such as lockdowns (which are detrimental to the social lives of younger cohorts), and why countries like China implemented more stringent measures.

Irrespective of country-specific reactions to Covid-19, research shows that differences in the social value of the older population are found to affect the health and life expectancy of individuals. Indeed, people with high self-perception are found to live on average 7.5 years longer than their lower self-perception counterparts (Levy et al. 2002). Similarly, other studies show that 35% of British society has experienced age discrimination (or ageism), which gives rises to lower health and wellbeing (Jackson et al, 2019). Hence, ageism, which has a more important bite during crises such as the current Covid-19 pandemic, has detrimental effects on the wellbeing of the population. When part of the population is locked down to protect mainly the wellbeing of older people, this needs to be kept in mind.
The precarious state of long-term care services costs lives
However, a delayed introduction of a lockdown is not the only way we reveal the low social value of older individuals. The Covid-19 pandemic has revealed how precarious is the funding and organisation of long-term care in a number of European countries. In the absence of affordable formal care, older individuals are informally cared for by family members (or go with unmet needs). Reliance on informal care explains the early expansion of the pandemic in countries with stronger family ties such as Italy, Spain, China and Korea.
Quarantines affect more severely older people, who are more likely to live alone and in need of care. Quarantine measures have had a large impact on caregiving. In many countries, caregivers have been forced to reside with older people in need to reduce the chance of contagion. But when older people are less disabled they are more likely to be left on their own, with unmet needs, or with the support of professional caregivers when available. However, many of these professionals were not regarded as key workers and in many cases could not provide their daily support.
Just like other long-term care services, nursing homes have experienced more than proportional fatalities. As of April, the coronavirus share of all deaths in nursing homes was 47% in France and 57% in Spain. A similar estimate (60%) is found in New York, whilst estimates are 45% in Italy. This is in part the result of limited investment in quality of care, in many cases resulting from tight budgets and recent austerity reforms that have left institutions short-staffed. This week, we have seen the announcement of pay rises for UK social care workers to address the situation, perhaps too late for the current crisis.
Lower priority for older people when health systems are congested costs lives
Another sign that older individuals exhibit a lower social valuation is the lower priority they receive when health care is congested amidst a pandemic, which means elderly people with health problems other than coronavirus are less likely to be treated when A&Es are at full capacity. This implicitly happens already, for instance, when roads are closed during marathons, which delays the time for ambulances to access a hospital, as Anupam B Jena finds. This applies to congested surgery theatres, when A&E and cancer surgeries are cancelled due to Covid-19, all of which overwhelmingly affect older people.
The lower priority of older patients when rationing health care has been a controversial issue in the literature. Since the 1970s, many medical ethicists (Harris, 1970) and economists (Williams, 1997) have adopted the view that when resources are limited, as they would in a pandemic such as Covid-19, one must consider the age of an individual. The basis for this is that there is a lifespan that we consider reasonable for an individual to live (a ‘fair inning’), and the health system, and more generally the government, should focus on ensuring that everyone is given an equal chance to attain a reasonable age — which might be country specific (say, 80 in the UK). Hence, individuals older than such a cut-off age would not be prioritised by intensive care units, and more generally whenever health care was rationed.
Certainty, such a criterion has significant detractors, as medical technology changes the age cut-off one can regard as ‘fair’, and because social values are not necessarily consistent with a ‘fair inning’ criteria. However, survey evidence suggests that in many European countries a significant share of the population supports prioritising younger individuals, which affects how the health system’s decision makers decide. Indeed, in Figure 2 below (reporting the average preference for a 30-year old compared to a 70-year old person when both need a heart operation), shows that although in most countries people think ‘age should make no difference’, over 40% of the population in the UK, France and Japan think that someone who is 30 years old should be prioritised by the health system.
In the context of the pandemic, British doctors are asked to consider patients’ age in critical care decisions. That is, they follow the Clinical Frailty Scale’ recommended by the National Institute for Health and Care Excellence (NICE), which takes the patient’s age into account. Similarly, the Italian health system prioritises younger patients following utilitarian premises that doctors should give priority to ‘saving a life’, and other European countries follow similar criteria. That implies a higher valuation for younger patients, who exhibit a higher capacity to benefit from critical care intervention. However, the nature of these choices is acknowledged by the latest ethics note of the British Medical Association, which states that “some patients may be denied intensive forms of treatment that they would have received outside a pandemic”. Hence, older individuals should be extra cautious so as not to fall sick in a pandemic.
Figure 2 – Suppose two equally sick people need the same heart operation. One is aged 30, the other 70. In your opinion who should get the operation first?
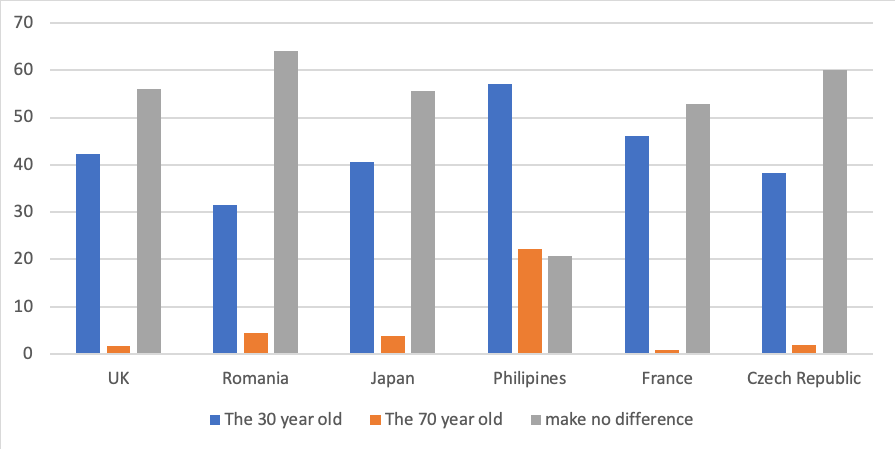
Source: International Social Survey Program (ISSP), 2011
Are older people safe from pandemics and its policy reactions?
Not only pandemics such as Covid-19 affect older people harder, but its policy reactions have revealed the lower social value of older populations, which explains why many have died alone or in isolation amidst delayed lockdowns. The underfunded system of long-term care services has turned nursing homes into ‘death homes’. And when faced with the need of critical health care, they have been given a lower priority. Yet, given that older individuals are an increasing share of our society, and that other pandemics are to come, we are left with the question: should countries revisit their priorities?
- This blog post appeared originally on LSE Business Review.
- Featured image via cozmicphotos, under a Pixabay licence
Please read our comments policy before commenting
Note: The post gives the views of its authors, not the position USAPP– American Politics and Policy, nor of the London School of Economics.
Shortened URL for this post: https://bit.ly/3eXsjuO
About the author
 Joan Costa-Font – LSE Health Policy
Joan Costa-Font – LSE Health Policy
Joan Costa-Font is an associate professor (reader) at LSE’s department of health policy. He is an economist affiliated with CESIfo in Munich and IZA, Bonn. He has been a Harkness fellow at Harvard University and a visiting fellow at UCL, Paris Dauphine University, Boston College, and Oxford University. He has taught at the University of Barcelona and the Università Cattolica in Milan. The core of his current research is on health economics.






It primarily reveals how much politicians value (or fear) the electoral influence of this age group!
Surely allowing the ‘get out’ of should not make a difference obfuscates the argument. You have one heart. Who gets it, the 30 or the 70? There is no such thing with this decision to make as “should not make a difference”. That sentiment is only for onlookers the actual decision-maker has to decide, so age WILL make a difference. Then, which one would YOU choose?