 Would-be NHS staff from overseas will shortly find it easier to secure permission to work in the UK. Doctors and nurses from the European Economic Area, who have helped to meet staff shortages in recent decades, may no longer have the right to do so. Parvati Raghuram (Open University) looks at how the NHS has depended on foreign workers since its creation.
Would-be NHS staff from overseas will shortly find it easier to secure permission to work in the UK. Doctors and nurses from the European Economic Area, who have helped to meet staff shortages in recent decades, may no longer have the right to do so. Parvati Raghuram (Open University) looks at how the NHS has depended on foreign workers since its creation.
The claim that the NHS would get an additional £350m per week if the UK quit the EU was arguably one of the most persuasive slogans of the Brexit campaign. The National Health Service has been one of the prides of the postwar social architecture and has come to be closely tied to British identity. Skilfully linking the NHS with Britishness was thus a winning strategy for Leave campaigners.
Commonwealth countries and the (Inter)National Health Service
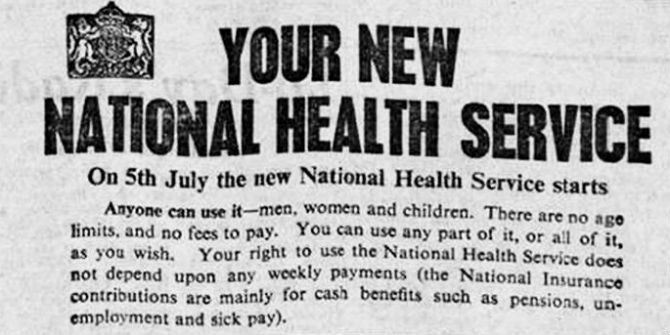
Migrant doctors from Europe, especially Jews who moved due to rising anti-Semitism in parts of Europe, had always formed a part of the medical profession in the UK. However, after the establishment of the NHS in 1948, many of the early flows were from the British Commonwealth countries. Training and work were inextricably intertwined through immigration regulations and the architecture of the health service, ensuring a steady supply of doctors (Table 1).
Thus. the National Health Service has always been an international health service. It has been populated by large numbers of migrant doctors who not only served the NHS but also constituted it, innovating and establishing it through specialist services in remote locations all over the UK. From the 1960s onwards a number of legislative changes were made to attract migrant doctors, who would come to populate the lower and middle parts of the pyramidal medical hierarchy. They did not contribute to a pre-existing NHS; rather they made the health service what it is today.
Table 1: Immigration rules affecting Commonwealth migrant doctors
| Year | Regulation |
|---|---|
| 1962 | Voucher system introduced |
| 1971 | Vouchers abolished; work permit system introduced |
| 1985 | Four-year permit-free training scheme introduced |
| 1997 | Nature of training available to non-EU migrants altered. Training typically takes five years, but all training posts had shorter stay periods |
| 2006 | Non-EU migration virtually closed |
The NHS and the EEA
Since the early 2000s there has been a shift towards recruitment from within the European Economic Area (Table 2). Freedom of movement within Europe led to an increase in the pool of migrant doctors, and in 2006 a dramatic shift took place – a virtual end to the migration of doctors who are third country nationals, i.e. those whose primary medical qualifications were obtained outside the EEA.
Immigration and EU workers: timeline
- Free movement until World War 1
- 1957: Reintroduction of freedom of mobility of workers through the Treaty of Rome
- 1973: UK joined European Community
- 1992: Freedom of mobility of citizens – Maastricht Treaty
- 2004 onwards: Expansion of the EU (ten countries joined in 2004; 2 in 2007; and 1 in 2013)
Migration regulations only tell half of the story. Professional workers like doctors can practice in the UK after registering and obtaining the appropriate licence. Under EU law doctors within the EEA cannot be discriminated against, but in June 2014 a new English language test was introduced for hose trying to obtain the licence to practice in the UK. This led to a reduction in the numbers of doctors obtaining a licence, compared to those who registered.
Table 2: Number of registered & licensed doctors in the UK by primary country of qualification
| PMQ country of origin | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
|---|---|---|---|---|---|---|---|---|
| Austria | 35 | 38 | 20 | 37 | 28 | 19 | 19 | 16 |
| Belgium | 43 | 36 | 36 | 22 | 37 | 31 | 35 | 45 |
| Bulgaria | 166 | 139 | 129 | 94 | 89 | 20 | 32 | 33 |
| Croatia | 1 | 2 | 3 | 23 | 110 | 24 | 23 | 25 |
| Czech Republic | 116 | 141 | 128 | 124 | 102 | 60 | 80 | 103 |
| Denmark | 30 | 20 | 17 | 16 | 25 | 7 | 14 | 7 |
| Estonia | 13 | 7 | 10 | 9 | 12 | 4 | 5 | 10 |
| Finland | 13 | 7 | 10 | 9 | 12 | 4 | 5 | 10 |
| France | 41 | 51 | 50 | 72 | 72 | 15 | 29 | 21 |
| Germany | 195 | 153 | 129 | 138 | 135 | 57 | 80 | 70 |
| Greece | 282 | 365 | 524 | 465 | 406 | 123 | 171 | 169 |
| Hungary | 207 | 186 | 175 | 125 | 89 | 44 | 57 | 63 |
| Iceland | 5 | 5 | 1 | 5 | 1 | 2 | 1 | 1 |
| Ireland | 129 | 145 | 137 | 170 | 174 | 242 | 244 | 241 |
| Italy | 370 | 386 | 425 | 610 | 744 | 124 | 137 | 137 |
| Latvia | 59 | 25 | 26 | 22 | 18 | 14 | 11 | 21 |
| Lithuania | 71 | 45 | 38 | 38 | 44 | 8 | 13 | 26 |
| Malta | 20 | 23 | 42 | 39 | 40 | 24 | 48 | 62 |
| Netherlands | 43 | 57 | 86 | 106 | 114 | 72 | 98 | 72 |
| Norway | 3 | 6 | 3 | 5 | 12 | 3 | 3 | 2 |
| Poland | 158 | 113 | 137 | 163 | 173 | 82 | 95 | 123 |
| Portugal | 48 | 64 | 92 | 82 | 104 | 47 | 30 | 54 |
| Romania | 677 | 449 | 288 | 276 | 263 | 108 | 170 | 164 |
| Slovakia | 40 | 40 | 49 | 44 | 57 | 17 | 28 | 29 |
| Slovenia | 7 | 3 | 17 | 10 | 15 | 3 | 6 | 11 |
| Spain | 124 | 159 | 264 | 323 | 247 | 49 | 67 | 65 |
| Sweden | 21 | 25 | 22 | 21 | 22 | 11 | 23 | 15 |
| Switzerland | 29 | 27 | 37 | 37 | 28 | 10 | 17 | 28 |
And back again to the Commonwealth?
Ten years later the tables turned as the UK voted to leave the EU. This led to large drops in the number of some health professionals such as nurses, although the full effects are yet to be documented across the sector. Growing staff shortages in some parts of the health sector are causing concern that the EEA will no longer serve the health workforce requirements of an ageing and rising population and its attendant demands for health care.
Although some areas such as emergency medicine, paediatrics and psychiatry have almost always been on the list of shortage specialties, and are allowed to recruit internationally, shortages are now more widespread. Moreover, the cap on Tier 2 visas (previously the Work Permit category) from outside the EEA to a maximum of around 20,000 per year across all the professions – alongside the demand from some other sectors such as IT for these visas – meant that many areas of the health service remain understaffed. NHS bosses have claimed that this significantly affects their ability to deliver healthcare safely and have pressed for the removal of the cap. The Home Secretary has now capitulated to these demands. What is clear is that the NHS, as ever, struggles to remain national.
Yet this internationalism of the NHS is only one exemplar of the UK’s position within a world of connections – with Europe and with other countries, including the Commonwealth. Only when the power and necessity of these connections – and their role in making the UK what it is today – is recognised will anti-immigration arguments and sentiments about Europeans and non-Europeans alike be challenged.
This post represents the views of the author and not those of the Brexit blog, nor the LSE.
Parvati Raghuram is Professor of Geography and Migration at the Open University.






“Only when the power and necessity of these connections – and their role in making the UK what it is today – is recognised will anti-immigration arguments and sentiments about Europeans and non-Europeans alike be challenged”
The inference that those who wish to see immigration controlled have a problem with highly qualified professionals coming here to work, either in the NHS or elsewhere, is a bogus one and is offensive to say the least.