Working out the trade-offs between saving lives and the economic damage of lockdown is complex. Marc Fleurbaey (Princeton), Hélène Fleurbaey (National Institute of Science and Technology) and Richard Bradley (LSE) have developed a model showing how different interventions can change the course of the pandemic. They conclude that the length of lockdown and early testing are crucial factors.
Should the current lockdown be extended? Should social distancing measures be maintained until the arrival of a vaccine? Would it be better to conduct large-scale testing in the way that South Korea has? Don’t all of these measures impose a risk of excessive economic cost? What is the overall effect of these measures on the wellbeing of the population?

Answers to these questions require an understanding of the different factors driving the pandemic, its effect on the economy and our wellbeing, and of how interventions change the nature and magnitude of these effects. We developed a model simple enough to be implemented in an Excel spreadsheet and which can be downloaded. Users can modify the main parameters of the model (the transmission rate of the virus, the ratio of deaths to infections, cautionary behaviour by the public, critical care capacity and the monetary values attributed to avoidance of loss of life and wellbeing) as well as construct different abstract policies, by setting the duration and frequency of lockdowns and the amount of testing conducted. The model then generates a comparison between different policies in terms of the number of lives saved (and social wellbeing preserved) and the estimated economic cost. Currently it can be used for the UK, the USA, France, Belgium and Guinea.
Too much uncertainty still exists about many of the inputs to use the model to make precise predictions, but it can nonetheless be used to get a better qualitative understanding of the causal mechanisms driving the pandemic and the effects of interventions designed to slow or stop it. It also enables us to better assess the trade-offs between the benefits of suppression and/or testing measures and their economic costs and to explore the robustness of policy conclusions to changes in the values of key parameters.
Here are some lessons that emerge from our own use of the model, based on a comparison between a benchmark case, in which individuals spontaneously social distance to some degree, and a suppression policy case based on enforced social distancing and growing use of testing. All the figures cited below refer to the UK model, though qualitatively the lessons are the same in all the countries studied.
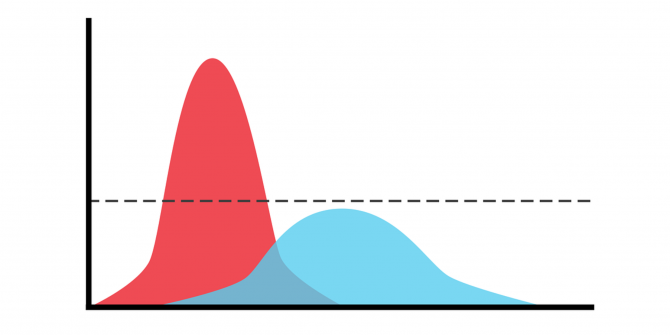
First of all, the model confirms that “flattening the curve” is essential because hospital capacity would be overwhelmed in the event of a sudden wave of patients. The significance of this factor depends on the difference between mortality rates for patients in hospital care and for untreated patients (whether or not COVID-19 infection is the cause of death). Although we lack precise figures for this difference, the Italian experience suggests that it is likely to be large.
Secondly, the difference between the projected course of the pandemic with and without a policy of suppression is considerable. Total mortality differs by a factor of nearly five. Those who claim that the suppression policies were unnecessary and that without them the final number of deaths would not be very different from a powerful seasonal flu are quite wrong. With the characteristics of the virus as estimated by the Imperial College team on UK data, there could have been in excess of 500,000 deaths in the UK, even taking into account the social distancing undertaken spontaneously (i.e. without official pressure) by the population as fear of the pandemic increases.
Thirdly, the model shows how the shape of the pandemic curve is very sensitive to the duration of suppression. Stopping suppression several weeks too early can change everything in subsequent months, and even increase final mortality by about 50% to 80% depending on the contagiousness of the virus. But extending it too long is also dangerous because it can leave us with a large number of people without immunity, contributing to a second wave of infections. These opposing considerations reflect the fact that the virus needs two things to thrive: a large number of infectious people to spread it and a large number of people not immunised to host it.
Simulations also reveal that the difference between a quick suppression of the contagion wave, as in Korea or China, and a prolonged and extensive wave, as in Europe or the United States, can depend on very small variations in the intensity and length of lockdown and the build-up of testing capacity. This is because when the lockdown policy brings the number of new cases to a manageable size, testing and contact tracing operations can then take over and further break the chain of transmission of the virus. Like a fire that must be quashed quickly before it gets too large, the pandemic has to be firmly and rapidly suppressed and for long enough. Half-hearted suppression measures, ironically, can have worse economic effects than brutal ones.
Fourthly, the model shows the value of testing people early to reduce the period during which they are contagious and in contact with others. If the exposure to the virus that infectious people impose on their contacts could be gradually reduced by up to 50%, this would have significant benefits, allowing the final mortality to be halved. Moreover, the economic cost of this policy is much less than that of the shutdown caused by widespread and indiscriminate confinement.
Finally, the model proposes an assessment of the societal cost of the crisis, integrating both mortality and economic costs, as well as social inequalities in the face of mortality and loss of income. To obtain a projection that is sensitive to inequalities, the model estimates the lifetime wellbeing of different social categories (income quintiles) in the two cases and allows for choice of the level of priority to give to disadvantaged people. Higher priority values give more favourable assessments to health systems that cover the less wealthy (involving less unequal mortality between social categories) and to economic policies that distribute the cost of containment more equitably.
What do the numbers say? The prevailing policies of suppression seem to have been well worth it, although much depends on the value attributed to the life years lost and the long-term economic cost. A rough calculation of the number of years of life that would have been lost if we had followed the benchmark policy, when each life-year is valued at three times per capita GDP (a commonly used threshold for the cost-effectiveness of health interventions), gives a loss due to mortality equivalent to 20% of one year of GDP. This seems likely to be greater than the relative GDP loss due to suppression measures (keeping in mind that the benchmark scenario also entails GDP losses due to the economic effects of spontaneous social distancing). On the other hand, if a life year is valued at one times per capita GDP (as NICE does for instance) then this conclusion can no longer be drawn.
Putting a figure on the value of years of life lost seems shocking at first glance, but it is necessary for making public safety trade-offs – trade-offs that each of us makes when deciding to accept the risks of everyday life. And, in view of the sensitivity of policy assessments to this figure, it is essential that the way in which life years are valued is subject to thorough discussion.
The views expressed in this text are those of the authors and do not reflect in any way the official position of Princeton University, LSE or NIST.





Have you taken into account the very low effect on the population under 50yrs of age who are in good health ? They are almost immune to the serious implications of CV19.
So I argue that under 50’s should ignore lockdown. They can keep the ecconomy alive without significant risk to life. The majority of scoiety would be back to normal, schools, shops, resturants. etc. There would be no need for “social distancing” and that would lead to herd immunity in the group.
People over 50 are high risk, and should be kept away from this population