
 Americans lead shorter and less healthy lives than people in other high-income countries. Is this US health disadvantage specific to some US populations, diseases, or particular age groups? And what explains these variations in the length and quality of life between Americans and other high-income countries? Mauricio Avendano and Ichiro Kawachi review the evidence and find the American health disadvantage begins at birth and extends across the life-course, and it is particularly marked for American women and for regions in the US South and Midwest. They propose explanations that include differences in health care, individual behaviors, socioeconomic inequalities, and the physical and the built environment. However, crucial differences in social policy between the US and other high income countries may also underlie an important part of the US’ health disadvantage.
Americans lead shorter and less healthy lives than people in other high-income countries. Is this US health disadvantage specific to some US populations, diseases, or particular age groups? And what explains these variations in the length and quality of life between Americans and other high-income countries? Mauricio Avendano and Ichiro Kawachi review the evidence and find the American health disadvantage begins at birth and extends across the life-course, and it is particularly marked for American women and for regions in the US South and Midwest. They propose explanations that include differences in health care, individual behaviors, socioeconomic inequalities, and the physical and the built environment. However, crucial differences in social policy between the US and other high income countries may also underlie an important part of the US’ health disadvantage.
Life expectancy gains in the US have not kept pace with gains in other high-income countries. In 2012, life expectancy in the US ranked 32 worldwide, below most other industrialized nations. Americans also experience higher rates of disease, injury and health-damaging behaviors than men and women in other high-income countries. The US health disadvantage emerged during the second half of the 20th century and has steadily grown, which is remarkable given that this coincided with a period of unprecedented economic growth and stability in the US. Using evidence from new research, we argue that next to Americans´ poorer access to healthcare and unhealthy lifestyles, crucial differences in American social policies may be responsible for an important share of the differences in health and life expectancy between the US and other high-income countries.
As Figure 1 illustrates, between 1960 and 2008, gains in life expectancy at birth ranged from 15.9 years in Japan to only 6.6 years in Denmark among women; and from 15.1 years in Portugal to 6.1 years in Denmark among men. US gains in life expectancy (7.5 years for women and 9 years for men) have been only about half of those in the best performing country. Next to the US, Denmark, the Netherlands and Norway have had comparatively modest gains in life expectancy, while women in Japan and Southern Europe (Portugal, Spain and Italy) have enjoyed the largest gains.
Figure 1 – Life expectancy at birth in the United States and in 16 other OECD countries, 1960–2010.
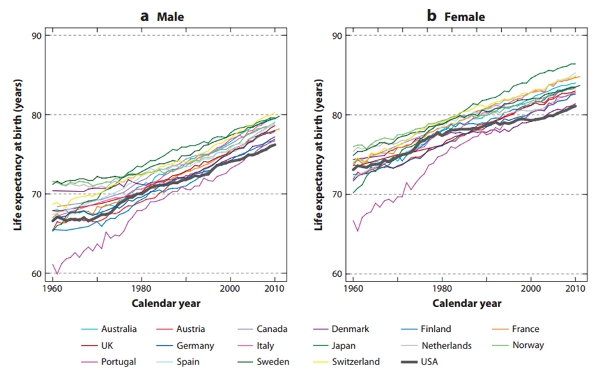
Source: Avendano, Mauricio and Kawachi, Ichiro (2014) Why do Americans have shorter life expectancy and worse health than do people in other high-income countries? Annual Review of Public Health, 35 (1). pp. 307-325.; OECD Health Data, OECD Health Statistics (Database)
One possibility is that these differences in mortality are driven by one or two specific causes of death that are particularly high in the US. We find that this is not the case: Mortality from many causes, including infectious diseases, complications of pregnancy; childbirth, conditions originating in the perinatal period, ischemic heart disease, diabetes and nervous system diseases are higher in the US than in nearly all other OECD countries. The US health disadvantage is not limited to mortality but extends to many other non-fatal health outcomes: Americans have higher prevalence of low birth weight, traffic injuries and HIV. Older Americans also report a higher prevalence of heart disease, stroke, hypertension, diabetes, obesity, lung disease and limitations with basic instrumental activities of daily living (IADL) than their European counterparts. Paradoxically, Americans are more likely to rate their own health as good compared to Western Europeans, but this appears to be driven by the fact that Americans are more ‘optimistic’ in general than people in other high-income countries.
What are the explanations for these marked differences in health between the US and other high-income countries? It is tempting to conclude that Americans have poorer health because some Americans have less access to high-quality care than, for example, European populations. There is, however, at best mixed evidence for this hypothesis. In general, the US does not seem to have systematically worse quality of care than other high-income countries, and in addition, both insured and uninsured Americans, as well as rich and poor Americans, appear to experience poorer health and higher mortality than Europeans. For example, excess deaths from violent causes (homicides, suicides, accidents) can hardly be attributable to lack of health care, suggesting that other mechanisms may be at play. It is now widely believed within public health that the main contributors to the onset of disease operate largely outside the influence of medical care.
Other explanations include individual behaviors, notably tobacco smoking, particularly among women. While Americans today smoke less than people in most other high-income countries, the smoking epidemic started earlier and reached a higher peak in the US than in other countries, particularly among women. Current mortality reflects smoking trends two to three decades earlier, and it is estimated that smoking explains about two fifths of the difference in male life expectancy beyond age 50 between the US and other high-income countries, and over three quarters of the difference in female life expectancy beyond age 50. Higher obesity rates and worse dietary habits may also contribute to these differences. However, smoking does not explain why young Americans have poorer health and worse mortality, because young Americans have smoked less than young adults in other OECD countries. Smoking is thus at best only one among several factors explaining the US health disadvantage. In general, an explanation that focuses exclusively on behavioral differences is impoverished by its focus on “proximal” individual choices.
The consistency of the US health disadvantage across the whole spectrum of disease and population suggest that explanations may need to be sought in upstream policies that differ crucially across the US and other high-income countries. While still a field in development, new research shows that social policies, such as childcare and early childhood policies, retirement policies, and education policies, may be causally linked to health. Because the US is often an outlier in some of these policies, we hypothesize that the crucial differences in some of these social policies may underlie differences in health and life expectancy between the US and other high-income countries.
Early childhood interventions appear to bring important health benefits, especially among disadvantaged children, and they are less accessible to American children than they are to children in many European countries. Studies indicate that early education programmes do not only improve educational outcomes but also lead to higher immunizations and height-for-age, and reduce child mortality at ages five to nine.
The US spends more on public school education than most other OECD countries, but American students perform around or below the OECD average. There are moreover substantial disparities in the quality of public schooling (e.g. reflected by student-teacher ratios) across communities in the United States, which are partly driven by residential segregation and the financing of the public school system by local property taxes. Education policies such as compulsory schooling laws have been shown to have long-run effects on health and mortality. Other policies, such as education grant aid programmes, have increased schooling completion and college attendance, and may also bring health benefits.
The US stands out for its weaker employment protection laws compared to other OECD countries. Social policies to protect workers who become ill or displaced, as well as maternity leave policies, are modest in the US in comparison to most European countries. Programmes to support working parents are also substantially less comprehensive in the US. In 2011-2012, the duration of fully-paid maternity and parental leave was 45 weeks in France, 46 weeks in Sweden, and 21 weeks in the Netherlands, compared to none in the United States.
Poverty rates are considerably higher in the US than in other OECD countries, particularly among children. In 2010, 21% of children in the United States lived in poverty, compared with 11% in France, 10% in the United Kingdom, and 8% in Sweden. These differences partly reflect the fact that cash minimum-income benefits are considerably lower in the US than in most other OECD countries. There is evidence that income transfer programmes have important health effects on low-income mothers and their children. For example, expansions of the Earned Income Tax Credit may have led to increased birth weight and reduced maternal smoking. Similarly, pregnancies exposed to the Food Stamps program had better birth outcomes than pregnancies unexposed, particularly among African American mothers.
Many European countries offer generous housing benefits for rental accommodation for families in need. By contrast, there is no US Federal programme for housing assistance, with only some states delivering programmes targeted to very low income households. The health impact of housing policies is poorly understood, but evidence from studies such as the Moving to Opportunity experiment suggests that housing itself is important to health.
Our review leaves little doubt that the Americans have poorer health and shorter life expectancy than other high-income countries. Public policies on early childhood, education, employment, income support and housing might influence health and mortality. These programmes are less comprehensive in the US than in most European countries, and may explain part of the US health disadvantage relative to other OECD countries. A better understanding of how social policies causally influence health is crucial to disentangling why the economic advantage of the US since the beginning of the post-war was not matched by a corresponding health advantage, but was in fact accompanied by less prosperous improvements in population health than in other high-income countries.
- This article is based on the paper ‘Why Do Americans Have Shorter Life Expectancy and Worse Health Than Do People in Other High-Income Countries?’ in the Annual Review of Public Health.
- Featured image credit: Credit: “The Stethoscope” (CC BY-NC 2.0) by Alex E. Proimos
Please read our comments policy before commenting.
Note: This article gives the views of the author, and not the position of USApp– American Politics and Policy, nor of the London School of Economics.
Shortened URL for this post: http://bit.ly/1gjiFCs
_________________________________
 Mauricio Avendano – LSE Health and Social Care
Mauricio Avendano – LSE Health and Social Care
Mauricio Avendano is Principal Research Fellow at LSE Health and Social Care. He is an epidemiologist with an interest in the causal impact of social and economic policies on health from a cross-national comparative perspective. He has been closely involved in the design and coordination of the health module of the Survey of Health, Ageing and Retirement in Europe (SHARE), a comparative study of 18 countries examining the links between health and the social and economic dimensions of life.
_
 Ichiro Kawachi – Harvard School of Public Health
Ichiro Kawachi – Harvard School of Public Health
Ichiro Kawachi is a Professor of Social Epidemiology, and Chair of the Department of Social and Behavioral Sciences at the Harvard School of Public Health. He has published over 400 articles on the social and economic determinants of population health.






